Virtual Library
Start Your Search
Ke-Neng Chen
Moderator of
-
+
OA10 - Sophisticated TNM Staging System for Lung Cancer (ID 136)
- Event: WCLC 2019
- Type: Oral Session
- Track: Staging
- Presentations: 9
- Now Available
- Moderators:Ke-Neng Chen, Pedro Lopez De Castro
- Coordinates: 9/09/2019, 14:00 - 15:30, Toronto (1985)
-
+
OA10.01 - Impact of Pre-Ordered Staging Tests on Timeliness of Lung Cancer Diagnosis and Staging: A Quality Improvement Initiative (Now Available) (ID 483)
14:00 - 15:30 | Presenting Author(s): Monica Lynn Laginha Mullin | Author(s): Audrey Tran, Christine Noseworthy, Christopher J. L. Stone, Christopher M Parker, Genevieve C Digby
- Abstract
- Presentation
Background
Timely care for patients undergoing evaluation for suspected lung cancer (LC) is critical to optimize clinical outcomes and minimize patient anxiety. We identified delays in local LC evaluation pathways and sought to improve the timeliness of care provided by the Lung Diagnostic Assessment Program (LDAP), a rapid assessment clinic. We launched a Quality Improvement (QI) initiative consisting of Standardized Triage Pathways (STP) with pre-ordered staging tests for LDAP-referred patients with a high suspicion of LC and seek to evaluate the impact on timeliness of care.
Method
Data were collected retrospectively for all LDAP-referred patients to establish baseline (January - April 2018) and prospectively for improvement (May - October 2018), including: LDAP referral date, triage pathway, pre-ordered tests (PET, CT/MRI brain) including date of completion, and reasons for not completing pre-ordered testing. Mean data are reported, with significance determine by special cause variation using Statistical Process Control (SPC) XbarS charts; unpaired t-tests assess for differences between independent groups.
Result
We reviewed 553 consecutive LDAP referrals (185 baseline, 368 post-STP). Compliance with STP and pre-ordered testing for patients with suspicion of LC improved to 100% and 93%, respectively. Post-STP, mean time from referral to PET decreased from 40.5 to 26.0 days, significant by SPC, and was 21.8 days for patients completing pre-ordered testing (p=0.0001). Time from referral to CT/MRI Brain decreased from 35.8 to 19.9 days, significant by SPC, and was 18.5 days for patients completing pre-ordered testing (p=0.0001). While there was a non-significant trend to improvement in time from referral to diagnosis (41.4 to 30.4 days), the improvement was significant for patients completing pre-ordered testing (28.4 days, p =0.0001). Of the 166 (45%) LDAP-referred patients triaged to receive pre-ordered testing, 134 (80.5%) completed pre-ordered tests. Those completing pre-ordered tests experienced more timely care, on average, than those who did not: mean time from referral to PET was 13.9 days faster (p=0.0001), referral to CT/MRI Brain was 15.9 days faster (p=0.0001), and referral to diagnosis was 10.2 days faster (p=0.0004). Main patient barriers to completing pre-ordered testing were preference for physician consultation prior to testing, (10, 31.3%), and barriers regarding travel and cost, (6,18.8%).
Conclusion
A standardized triage process with pre-ordered staging tests at the time of LDAP referral is associated with improved time from referral to completion of staging tests and diagnosis. Strategies to improve compliance with pre-ordered testing are ongoing, including collaboration with primary care physicians and nurses to support patients and navigate barriers.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA10.02 - Recommended Change for N Descriptor Proposed by the IASLC: A Validation Study from a Single-Center Experience (Now Available) (ID 2117)
14:00 - 15:30 | Presenting Author(s): Byung Jo Park | Author(s): Tae Ho Kim, Sumin Shin, Hong Kwan Kim, Yong Soo Choi, Jhingook Kim, Jae Ill Zo, Young Mog Shim, Jong Ho Cho
- Abstract
- Presentation
Background
The International Association for the Study of Lung Cancer (IASLC) recently proposed changes for N descriptor based on the location and number of involved lymph node stations. The aim of our study was to evaluate the discriminatory ability and prognostic performance of the proposed N descriptor in a large independent non-small cell lung cancer (NSCLC) cohort.
Method
IASLC proposals include: a classification of N descriptor by combining the present nodal categories and number of involved lymph node stations into: N0; single-station N1 (N1a); multiple-stations N1 (N1b); single-station N2 without N1 involvement (N2a1); single-station N2 with N1 involvement (N2a2); multiple-stations N2 (N2b) and N3. A total of 1128 patients who underwent major pulmonary resection for pathologic N1 or N2 NSCLC between 2004 and 2014 were analyzed in this study. survival analysis was performed using Cox proportional hazard model to assess the prognostic significance of the N descriptor.
Result
From 2004 to 2014, 7437 patients were operated on for non-small-cell lung carcinoma (NSCLC). Among those, patients who underwent preoperative treatment for stage IIIA-N2 NSCLC were excluded (N=-698, 9.4%). Patients who were confirmed as pathologic N1 (N=676) or N2 (N=452) after surgery were included in this study. Invasive mediastinal staging (EBUS or mediastinoscopy) was done in 614 patients (54.4%). After surgery, adjuvant treatments were performed in 901 patients (81.7%). The mean total number of dissected lymph node was 25.7 ± 11.0, and the mean number of involved (metastatic) lymph node was 3.0 ± 3.2. The 5-year overall survival rate was 64.7 % in N1a, 57.1% in N1b, 68.0% in N2a1, 50.1% in N2a2, and 46.7% in N2b. Based on our study about the overall survival and recurrence-free survival, N2a1 is not clearly divided into N1a and N1b is not clearly divided with N2a2.
Conclusion
Based on the proposed N stage classification by combining the LN station number with the proposed anatomic location in IASLC, all 5 groups were not clearly identified. According to our analysis, it would be better to classify similar prognostic group as 3 or 4 group to divide the group. The new N classifications should be considered for future revisions of TNM staging system for lung cancer.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA10.03 - Macroscore: A Prognostic Model for Supplementing the TNM Stage in Resectable Non–Small Cell Lung Cancer (Now Available) (ID 630)
14:00 - 15:30 | Presenting Author(s): Rui Mao | Author(s): Mu Li, Chang Chen, Ran Wang, Haoyue Guo, Jiani Gao
- Abstract
- Presentation
Background
We aim to establish a prognostic model based on the macrophage status to supplement the TNM stage and increase the predictive accuracy for the prognosis of NSCLC patients.
Method
The macrophage infiltration at the center of the tumor and its invasive margins in stage I to IIIA NSCLC patients (n=368) was evaluated, and a Macroscore model was constructed (Low/Intermediate/High). The relationship between the Macroscore and the clinical outcome was analyzed and validated by 2 additional cohorts.
Result
The Macroscore was significantly associated with disease-free survival rates and overall survival rates at each TNM stage (all p < .0001). The TNM stage could not, however, determine survival rates in patients with the same Macroscore (figure 1). In patients experienced a 5-year event, the Macroscore is usually in high level (26.0%-53.1%). Patients have not experienced a 5-year event usually have a low Macroscore (71.7%-84.8%), regardless of the TNM stage (figure 2). Furthermore, the Macroscore could improve the area under the curve values for the DFS and OS; the values of DFS increased from 0.651 for the TNM system model to 0.822 for the TNM stage plus Macroscore model.

Conclusion
The Macroscore provides an accurate prediction of the clinical outcome in resectable NSCLC tumors, and it complements the prognostic value of the TNM stage.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA10.04 - Discussant - OA10.01, OA10.02, OA10.03 (Now Available) (ID 3767)
14:00 - 15:30 | Presenting Author(s): Valerie W. Rusch
- Abstract
- Presentation
Abstract not provided
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA10.05 - Which Is Better for TNM Stage Assessment Among Whole-Body MRI and PET/MRI at 1.5 Tesla and 3 Tesla and FDG-PET/CT in Non-Small Cell Lung Cancer? (Now Available) (ID 910)
14:00 - 15:30 | Presenting Author(s): Yoshiharu Ohno | Author(s): Kota Aoyagi, Masao Yui, Daisuke Takenaka, Takeshi Yoshikawa
- Abstract
- Presentation
Background
Accurate tumor staging is essential for choosing the appropriate treatment strategy for non-small cell lung cancer (NSCLC) patients. In 1990s, positron emission tomography (PET) or PET combined with CT (PET/CT) using 2-[fluorine-18]-fluoro-2-deoxy-D-glucose (FDG) were suggested as useful for TNM stag evaluation in NSCLC patients in routine clinical practice. Since 2007, whole-body magnetic resonance imaging (MRI) with diffusion-weighted imaging (DWI) at 1.5T or 3T systems and PET/MRI have been continuously testing in this setting. Moreover, PET fused with MRI (PET/MRI) with FDG has been suggested as a new tool for TNM stage and postoperative recurrence evaluations since 2015. However, all PET/MRI has been generated by MRI at 3T MR system and not tested that at 1.5T system. No one reported direct comparisons for TNM staging capability among whole-body MRI and PET/MRI at 1.5T and 3T systems and PET/CT in NSCLC patients. We hypothesize that whole-body MRI and PET/MRI at 1.5T and 3T MR systems have better potential for TNM stage assessment than whole-body FDG-PET/CT in NSCLC patients. The purpose of this study was to prospectively and directly compare TNM stage classification capability among whole-body MRI and PET/MRI at 1.5 and 3T MR systems and PET/CT in NSCLC patients.
Method
104 consecutive pathologically diagnosed NSCLC patients (62 men, 42 women; mean age 71 years) prospectively underwent whole-body MRI at 1.5T and 3T systems, integrated PET/CT, and surgical, pathological and/ or follow-up examinations. Final diagnoses of T, N and M factors and clinical stage in each patient were determined according to all examination results. Then, each factor and clinical stage were visually assessed on both whole-body MRIs, PET/MRIs and PET/CT with contrast-enhanced brain MRI. Kappa statistics were used to determine agreements for assessment of all factors and clinical stage with final diagnoses, and McNemar’s test was used to compare each diagnostic accuracy among all methods.
Result
Conclusion On each factor and clinical stage assessments, agreements between all methods and final diagnosis were substantial or almost perfect (0.60<κ<0.98). Diagnostic accuracies of N factor and clinical stage on whole-body MRI as well as PET/MRI at both field strengths were significantly higher than those of PET/CT (p<0.05).
On each factor and clinical stage assessments, agreements between all methods and final diagnosis were substantial or almost perfect (0.60<κ<0.98). Diagnostic accuracies of N factor and clinical stage on whole-body MRI as well as PET/MRI at both field strengths were significantly higher than those of PET/CT (p<0.05).
Whole-body MRIs and PET/MRIs at 1.5T and 3T systems have significantly better potential for N factor and clinical stage assessments than PET/CT in NSCLC patients.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA10.06 - Transition Patterns Between N1 and N2 Stations Discovered from Data-Driven Lymphatic Metastasis Study in Non-Small Cell Lung Cancer (Now Available) (ID 1499)
14:00 - 15:30 | Presenting Author(s): Xing Wang | Author(s): Nan Wu, Qitian Chen, Xiang Li, Quanzheng Li
- Abstract
- Presentation
Background
N staging process was essential for evaluation of outcome and indication of following adjuvant therapies in Non-small-cell lung cancer treatment. Various clinical observations on the potential transition patterns of lymph node drainage are reported, however, most of the previous conclusions were made by clinical physicians and focused on specific empirical transition patterns. The fact that there is no definitive and holistic map for lymphatic metastasis transition patterns, and the patients were suffering from either excessive nodes collection along with more damage, or insufficient nodes collection with potential recurrent risks.
Method
We perform complete lymph node examination of a total of 936 subjects diagnosed with NSCLC lung cancer. Lymph nodes sampling or dissection are performed according to NCCN guidelines.
A probabilistic model is developed due to the presence of these missing values. Using the maximum likelihood estimation and proximal gradient algorithm, the summarization of dataset is obtained, which were several explicit metastases and their corresponding probabilities. The metastasis graph is constructed from the summarization result with greedy algorithm and a given threshold. Besides, numerical simulation experiments are conducted to validate the stability of algorithms.
Result
Lymph node sites are shown as round circles according to their anatomical locations. The inferred transition paths are shown as edges connecting them. Edges colored in red are those consistently found in the left and right lung, and blue for unique nodes at each side thus cannot be compared, and black for different patterns between left and right lungs.
Closely connected intra-lobar (N1) nodes: strong connections among intra-lobar nodes (10~14). Over 78% among all the patients have more than 7 edges connecting the 5 intra-lobar nodes.
Jumping metastasis from N1 to N2 stations: We found that there exists several jumping metastasis at both sides of the lobes which has not been well-studied yet posing a challenge for the diagnosis and accurate staging (eg. 12 to 4, 13 to7, 11 to 2), revealing potential long-range transition pathways.
Correlation among N2 lymph nodes: We discovered the presence of certain metastatic groups, including node 5/6, 5/9, 7/9, 6/8 for left lung, and 2/4,2/7,7/9, 2/3p, 3p/7 for right lung.
Conclusion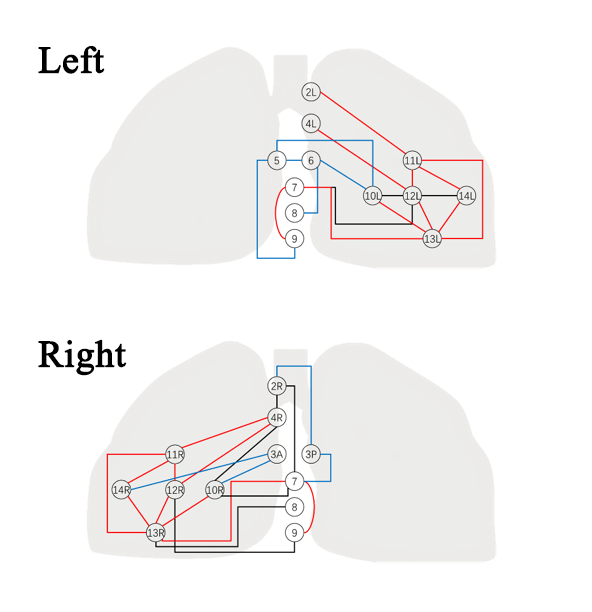
So we drew a map precisely to make a better understanding for metastatic pathways and provide a potential tool for the prediction of involved nodes pre/ or intro-operatively,so that an individualized surgical planning strategy could be made.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA10.07 - Concordance Between ROSE and Final Diagnosis in Patients Undergoing EBUS- TBNA for Non-Small Cell Lung Cancer Staging (Now Available) (ID 1123)
14:00 - 15:30 | Presenting Author(s): Cristina Caupena Auledas | Author(s): Mireia Martinez Palau, Bruno García Cabo, Teodora Pribic, Lluis Esteban Tejero, Francisco Perez Ochoa, Raquel Albero Gonzalez, Carme Ferrer Cassado, Pilar Forcada Guiu, Sandra Patricia Pontes De Sousa, Xavier Tarroch Sarasa, Jose Sanz Santos
- Abstract
- Presentation
Background
In patients with non-small cell lung cancer (NSCLC) undergoing mediastinal staging through endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) clinical decision making is based in rapid on-site evaluation (ROSE) findings. We aimed to analyze the accuracy of ROSE determining the rate of concordance between ROSE and final diagnosis.
Method
Prospective study that included patients undergoing EBUS-TBNA for NSCLC staging. Results of ROSE were compared with final diagnosis.
Result
Sixty-four patients were included and 637 lymph nodes (LN) were sampled: a median of 10 (IQR 8-12) LNs and a median of 5 (IQR: 4-6) nodal stations per patient were sampled. The diagnoses of ROSE were concordant with the final diagnoses in 612 (96.1%) cases and non-concordant in 25 (3.9%). There were 7 (1.2%) LNs in which the diagnosis of ROSE was non-malignant with a final diagnosis of malignancy. On the contrary, there was a single case (0.2%) in which the diagnosis of ROSE was malignant with the final diagnosis being normal LN. Considering final diagnosis as the gold standard, the sensitivity, specificity and overall accuracy of ROSE were 98.6, 97.2 and 98.5% respectively.
Table 1:
ConclusionDIAGNOSIS
ROSE
FINAL DIAGNOSIS
Non-diagnostic/
Inadequate
(82)
Benign/
Normal lymph node (520)
Malignancy
(36)
Non-diagnostic/
Inadequate
(70)
67
3
0
Benign/
Normal lymph node (526)
14
511
1
Malignancy
(42)
1
6
35
The preliminary diagnoses (ROSE) are concordant with the final diagnoses in a high percentage. Consequently, clinical decisions based on the ROSE can be taken with confidence.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA10.08 - Discussant - OA10.05, OA10.06, OA10.07 (Now Available) (ID 3768)
14:00 - 15:30 | Presenting Author(s): Akif Turna
- Abstract
- Presentation
Abstract not provided
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA10.09 - Clifton F. Mountain Lectureship Award for Staging (Now Available) (ID 3900)
14:00 - 15:30 | Presenting Author(s): Paula Antonia Ugalde
- Abstract
- Presentation
Abstract not provided
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.


