Virtual Library
Start Your Search
Tomasz Grodzki
Moderator of
-
+
OA06 - Refining Lung Cancer Screening (ID 131)
- Event: WCLC 2019
- Type: Oral Session
- Track: Screening and Early Detection
- Presentations: 8
- Now Available
- Moderators:Tomasz Grodzki, Lluis Esteban Tejero
- Coordinates: 9/09/2019, 11:00 - 12:30, Hilton Head (1978)
-
+
OA06.01 - Comparison Between Radiomics-Based Machine Learning and Deep Learning Image Classification for Sub-Cm Lung Nodules (Now Available) (ID 2810)
11:00 - 12:30 | Presenting Author(s): Calum Macaulay | Author(s): Ian Janzen, Saeed Seyyedi, Ronald Abraham, Sukhinder Kaur Atkar-Khattra, John Mayo, Ren Yuan, Renelle Myers, Stephen Lam
- Abstract
- Presentation
Background
New clinical challenges have arisen from the recent recognition for an improved mortality of cancers via lung cancer screening using LDCT. A particular challenge for physicians and CADx systems is the classification and prediction of behavior for sub-cm lung nodules that are frequently present in screening CT scans. By predicting and classifying the behavior of these small nodules, we can identify potential cancerous nodules into the earlier stages of malignancy making them more easily treatable.
Method
We have evaluated a multitude of image processing techniques to assist in CADx systems for these small nodules such as Radiomic feature-based machine learning algorithms (linear discriminant analysis) as well as leveraging pretrained convolution neural networks such as VGG19 and InceptionV3 using deep learning/transfer learning techniques. The linear discriminate Radiomic analysis (LDA) classified a sample of CT imaged nodules (n=514) using quasi-volumetric nodule data (images of the nodules from CT slices above and below the central slice) into three discriminate categories: cancerous (clinically confirmed, n = 140) versus resolved (not present in follow up CT scans, n=107) versus stable (a negligible change in shape, texture, size in multi year follow up CT scans, n=267). Each nodule was segmented from the original CT scan using an inhouse lung CT image segmenation routine. This routine generated 2167 discrete CT nodule images upon which 133 Radiomic shape and texture features were calculated.
Result
The LDA Radiomic analysis correctly classified the individual nodual sections with an accuracy of 75.1% (jackknife - leave one out result) using only 18 features predefined traditional image analysis features (4 shape feature(s), 14 texture feature(s)) for cancer vs resolved + stable nodules. Requiring that more than or equal to 50% of sections from a nodule be classified as cancer for the nodule to be classified as cancer individual nodules could be correctly classified with an 80% accuracy.
The leveraged pretrained networks (VGG19, and InceptionV3) trained using standard data augmentation and finetuning techniques, trained on this same quasi-volumetric image data as a binary classification task (malignant vs. benign nodules) achieved an average classification accuracy of 71% and 75% respectively through 10-crossfold validation.
Conclusion
Machine learning using 18 Radiomics features was able to classify 75.1% of the 2167 CT nodule images (up to 5 images/CT slices per nodule) and 80% of the nodules correctly. The best of the Deep Learning networks achieved almost equivalent results.
The image classification deep neural network results suggest the implementation of more advanced regularization and initialization deep learning techniques to further refine the decision boundaries for these pretrained networks might be benefitial. We believe the development of visualization neural network software to highlight the defining nodule features during classification would clinically assist in providing context clues for nodule diagnosis.
This work has been supported by TFRI project ref:1068
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA06.02 - The Role of Simulation Modeling in Shaping Lung Cancer Screening Policies in the US and Elsewhere (Now Available) (ID 1012)
11:00 - 12:30 | Presenting Author(s): Rafael Meza
- Abstract
- Presentation
Background
Models of the natural history of cancer have played an important role in shaping cancer prevention and control policies across the world. Notably, the US National Cancer institute (NCI) Cancer Intervention and Surveillance Modeling Network (CISNET) consortium has developed multiple such models and a modeling infrastructure that has supported the development of guidelines and policies for cancer screening and tobacco control in the US and elsewhere.
Method
The CISNET Lung models incorporate and synthetize smoking and lung cancer data from clinical trials, epidemiological studies and surveillance systems. These models have informed US screening guidelines. But important questions remain as screening programs are being implemented, such as the relative effectiveness of risk-based versus pack-year eligibility strategies or the potential of cessation programs within the context of lung screening.
Result
Simulation of the US 1950 and 1960 birth-cohorts show that for a given number of screens, risk-based screening programs lead in general to higher mortality reductions than pack-year based strategies. This is also true for LYG, but the difference is less pronounced. Independently of the program, adding cessation interventions at the point of screening leads to considerable gains in LYG, and to a lesser effect on deaths prevented. E.g., under current guidelines and a 40% screening uptake scenario, adding a cessation intervention at the time of first screen with a 15% success probability, could increase LYG by 140% and lung cancer deaths prevented by 28% (fig). But the actual gains would greatly depend on coverage and the cessation probability (fig).
Conclusion
Simulation modeling provides a framework to extrapolate findings from clinical trials and epidemiological studies into population outcomes. This has shown to be key to be able to refine and identify lung cancer prevention optimal strategies for a given setting. And to gather support among stakeholders to adopt and implement such strategies.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA06.03 - An Open Source Lung Screening Management System (Now Available) (ID 1467)
11:00 - 12:30 | Presenting Author(s): Claudia I Henschke | Author(s): Anthony P Reeves, Ricardo Avila, Drew Moghanaki, Artit Jirapatnakul, David F. Yankelevitz
- Abstract
- Presentation
Background
Starting in 1992, the Early Lung Cancer Screening Project (ELCAP) investigators developed the ELCAP Management System (MS) to ensure high quality care and follow-up of the first 1,000 ELCAP participants. The resulting Lancet publication in 1999 created worldwide interest in screening and an updated web-based ELCAP MS was updated to be web-based and provided free of charge to participating institutions, together with the I-ELCAP protocol.
Method
The ELCAP MS was designed to be comprehensive and rapidly capture information on each participant to be used by coordinators, navigators, nurses, radiologists, and other medical professionals to ensure appropriate follow-up and care. It provides rapid documentation of telephone or other inquiries, registering, scheduling screening appointments, reporting results, diagnosis of lung cancer, and treatment, and archives all CT images for integrated access of image and patient information. It has been iteratively updated through user feedback, and supports medical reimbursement requirements and continuous quality improvement to minimize harms of lung screening across International ELCAP (I-ELCAP) sites.
Result
More than 81,000 participants in 80 institutions worldwide have contributed their LDCT findings and images. The MS has provided efficient data collection for rigorous assessment of screening outcomes which has resulted in some 300 publications and abstracts for protocol updating, comparisons, and continuous quality improvement.
Having anticipated “open science”, the ELCAP MS has been translated into an open source MS that offers a reference standard for data elements (1,500 data fields, 267 required) for robust and efficient management of lung screening programs. This first open source translation has been adopted by the United States Veterans Administration (VA) and integrated into its VistA Electronic Healthcare System for deployment at 10 VA medical centers through a grant for VA Partnership to increase Access to Lung Screening (VA-PALS). The software is being certified by the Open Source Electronic Health Record Alliance (OSEHRA); source code is available on GitHub.
Automated quantitative tools have been developed for identification and characterization of nodules, emphysema, major airways, calcification scoring of coronary arteries, aortic valve, thoracic aorta, breast tissue, liver, bone, and image quality. These tools are integrated into the ELCAP MS, and in the future will provide automatically-generated quantitative LDCT reports.
Conclusion
The ELCAP MS and I-ELCAP protocol have helped define current global standards for lung screening. Its developers have now made the ELCAP MS publicly available through OSEHRA for support of lung screening programs of any scale throughout the world.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA06.04 - Discussant - OA06.01, OA06.02, OA06.03 (Now Available) (ID 3756)
11:00 - 12:30 | Presenting Author(s): Betty C Tong
- Abstract
- Presentation
Abstract not provided
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA06.05 - Evaluation of a Deep Learning-Based Automatic Classifier for the Classification of Perifissural Nodules (Now Available) (ID 1928)
11:00 - 12:30 | Presenting Author(s): Daiwei Han | Author(s): Marjolein A. Heuvelmans, Mieneke Rook, Monique D. Dorrius, Luutsen Van Houten, Noah Waterfield Price, Lyndsey C Pickup, Petr Novotny, Jerome Declerck, Matthijs Oudkerk, P.M.A Van Ooijen, Fergus Gleeson, Rozemarijn Vliegenthart
- Abstract
- Presentation
Background
Perifissural nodules (PFNs) comprise approximately 20% of screening-detected nodules and are almost certainly benign. Automatic PFN classification could therefore reduce the number of follow-up procedures required for nodule work-up. Prior work has shown some success in AI classification with limited datasets. Here we evaluate the performance of a new deep convolutional neural network (CNN) for PFN classification, trained on a dataset of nodules retrospectively collected from multiple European centers, including validation on an independent reader-study dataset.
Method
Data (1103 Patients, 1557 unique nodules and 3320 nodule images) were collected from three centers in the UK and the Netherlands. Each nodule was categorized into subtypes, including “PFN”, by on-site radiologists. Labels were reviewed centrally, overseen by a single clinician to ensure consistency between sites.
A CNN classifier was trained to produce a score that classifies nodules as (typical) PFN or not, using five-fold cross validation. The PFN classifier was developed by “transfer learning” from an existing benign-vs-malignant AI trained on the US National Lung Screening Trial.
To compare the CNN with human performance, independent validation was performed on a separate dataset of 158 benign patients (196 nodules/nodule images) from two of the sites. Three readers (two radiologists and a radiology resident) were asked to label each nodule as typical PFN, atypical PFN, or non-PFN. To match the AI training procedure, only the typical-PFN labels were used in the reader study, and compared to atypical/non-PFN classified nodules.
Model performance was evaluated by area under the ROC curve (AUC). For the independent validation, Cohen’s kappa was used to measure both the model’s agreement with reader consensus (at least 2 in agreement) and inter-reader agreement. For Cohen’s kappa calculations the CNN score was binarized using a threshold determined from the internal validation data.
Result
The mean cross-validated AUC on the internal dataset was 92% (95% CI = 90.6–92.9). For the independent dataset, the classifier labelled 61/196 (31%) as typical PFNs, and reader consensus gave 45/196 (23%). Versus reader consensus, the AUC of the CNN on the reader-study dataset was 96% (95% CI 93.3–98.4). Both the classifier–reader agreement [(k=0.74) 90%] and the inter-reader agreement [(k=0.64–0.79) 88%-92%] were substantial.
Conclusion
The performance of the PFN classifier is similar to that of radiologists and is within the inter-reader variability of radiologists. This demonstrates the potential utility of CNN-based systems for automatic PFN classification.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA06.06 - Independent Validation of a Novel High-Resolution Computed Tomography-Based Radiomic Classifier for Indeterminate Lung Nodules (Now Available) (ID 2862)
11:00 - 12:30 | Presenting Author(s): Tobias Peikert | Author(s): Fenghai Duan, Srinivasan Rajagopalan, Ron Karwoski, Aneri B Balar, Dhairya Lakhani, Sanja L Antic, Brian Bartholmai, Johnson Tucker, Pierre P Massion, Fabien Maldonado
- Abstract
- Presentation
Background
Optimization of the clinical management of incidentally- and screen-identified lung nodules is urgently needed to limit the number of unnecessary invasive diagnostic interventions, and therefore morbidity, mortality and healthcare costs. We recently developed and internally validated a novel radiomics-based approach for the classification of screen-detected indeterminate nodules, and present herein validation of this algorithm in an independent cohort.
Method
In a previous study, we developed a multivariate prediction model evaluating independent quantitative variables assessing various radiologic nodule features such as sphericity, flatness, elongation, spiculation, lobulation and curvature. Nodules between 7 and 30 mm of largest diameter were selected from the National Lung Screening Trial (n=726 indeterminate nodules, benign (n = 318) and malignant (n = 408)) were used to derive this model using least absolute shrinkage and selection operator (LASSO) method with bootstrapping method applied for the internal validation. Eight variables capturing vertical location, size, shape, density and surface characteristics were included with an optimism-correct area under the curve (AUC) of 0.94. For this study, an independent dataset of 203 incidentally-identified lung nodules obtained from the indeterminate pulmonary nodule registry at Vanderbilt University was identified. CT datasets were transferred to Mayo Clinic (Rochester, MN) for analysis. Nodules were segmented manually using the ANALYZE software (Biomedical Imaging Resource, Mayo Clinic, Rochester, MN), and radiomic analysis was performed using the 8-variable radiomic diagnostic algorithm derived from the NLST. The Brock model was also used to calculate probability of malignancy for all NLST and Vanderbilt nodules.
Result
Brock scores were calculated for 685 NLST nodules (excluded: interval cancers, n=12; missing values needed for Brock score, n=29). The AUC for the Brock score (AUC Brock) for NLST nodules was 0.83 which was inferior to the AUC for the radiomic model (AUC Radiomic =0.94, P<0.001). When the subset of intermediate pre-test probability of lung cancer was considered (Brock score > 10 but <= 60), the AUC Brock was 0.61 (95% CI: 0.54-0.68) whereas the AUC Radiomic was 0.88 (95% CI: 0.84-0.93). A total of 203 incidentally found pulmonary nodules with available clinical information and biopsy or surgery-proven histology identified in the Vanderbilt indeterminate pulmonary nodule registry, and all histology data and corresponding CT images were reviewed. CT images were transferred to Mayo Clinic for analysis. After exclusion of duplicate CT datasets, unanalyzable CT images and not identifiable nodules (n=27 cases), 176 nodules were segmented and analyzed, including 84 benign and 92 malignant nodules. The AUC was 0.89 (95% CI: 0.85-0.94). For comparison, the AUC Brock was 0.88 (95% CI: 0.83-0.94). When the subset of intermediate pre-test probability of lung cancer was considered (Brock score > 10 but <= 60), the AUC Brock was 0.76 (95% CI: 0.63-0.89) whereas the AUC Radiomic was 0.85 (95% CI: 0.74-0.95).
Conclusion
Our radiomic classifier demonstrates good performance characteristics on an independent retrospective validation dataset. If prospectively validated, integration into clinical decision making algorithm could significantly impact patient care.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA06.07 - Discrimination of Lung Invasive Adenocarcinoma with Micropapillary Pattern Based on CT Radiomics (Now Available) (ID 399)
11:00 - 12:30 | Presenting Author(s): Haihua Yang | Author(s): Yunyu Xu, Wenbin Ji, Liqiao Hou, Chao Zhou, Wei Wang, Suna Zhou, Feng-Ming Spring Kong
- Abstract
- Presentation
Background
To develop and validate the radiomics nomogram on the discrimination of lung invasive adenocarcinoma (IAC) with micropapillary pattern from non-micropapillary pattern lesion and improve the diagnostic accuracy rate of lung invasive adenocarcinoma with micropapillary pattern before operations and provide guidance for follow-up treatments.
Method
Forty-one pathologically confirmed lung invasive adenocarcinomas with micropapillary pattern from January 2014 to December 2018 were included. Eighty-two pathologically confirmed lung invasive adenocarcinomas without micropapillary pattern from January 2018 to December 2018 were collected. Select 86 patients (70%) randomly from the 123 patients as the primary cohort, and the other 37 patients (30%) were set as an independent validation cohort. Least absolute shrinkage and selection operator (Lasso) was used for feature selection based on contrast enhancement CT images and then radiomics signature building. ROC analysis and AUC were used to value the ability to identify the lung invasive adenocarcinomas with micropapillary pattern.
Result
According to GrayLevelCooccurenceMatrix3, Intensity Histogram and Shape, nine hundred and eighty-five radiomics features were extracted by IBEX. And after data pre-processing such as eliminating missing items, strong correlation variables and multicollinear variables, the features were reduced to 40 features. Based on Mann-Whitney U Test, 28 features were figured out from the 40 features. Then Lasso was used to reduce the features to 3 features (10-1clusterprominenc, -333-4clusterprominence, 8-1contrast) as the most meaningful discriminators to build the radiomics signatures (Table 1). According to SPSS21.0 binary logistic regression analysis, ROC analysis and AUC show that the radiomics signature have effective discrimination performance of lung invasive adenocarcinoma with micropapillary pattern from non- micropapillary pattern lesion (AUC=0.766) and it reflects better in the independent validation cohort (AUC=0.807) (Figure 1).
Table 1 Three characteristic prediction parameters in radiomics label
prediction parameter P value U value W value AUC 10-1clusterprominence <0.005 765.000 4168.000 0.772 -333-4clusterpromise <0.005 790.000 4193.000 0.765 8-1contrast <0.005 919.000 4322.000 0.727
Conclusion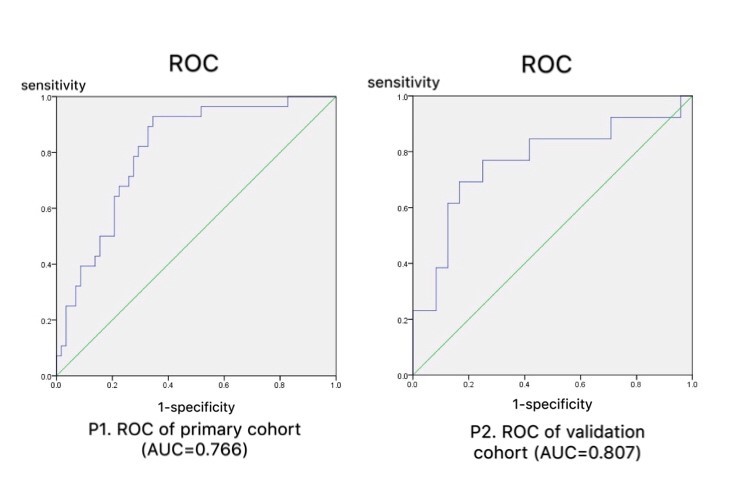
The radiomics signature established in this study have effective prediction of lung invasive adenocarcinoma with micropapillary pattern and non- micropapillary pattern lesion.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA06.08 - Discussant - OA06.05, OA06.06, OA06.07 (ID 3757)
11:00 - 12:30 | Presenting Author(s): Jamie Ostroff
- Abstract
Abstract not provided
-
+
OA13 - Ideal Approach to Lung Resection and Novel Perioperative Therapy (ID 146)
- Event: WCLC 2019
- Type: Oral Session
- Track: Treatment of Early Stage/Localized Disease
- Presentations: 9
- Now Available
- Moderators:Tomasz Grodzki, Kenji Suzuki
- Coordinates: 9/10/2019, 11:30 - 13:00, Toronto (1985)
-
+
OA13.01 - SPECS2 Lung Cancer Consortium Prospective Multicenter Validation of Prognostic Signature for Early Stage Squamous Lung Cancer (Now Available) (ID 2723)
11:30 - 13:00 | Presenting Author(s): Raphael Bueno | Author(s): David Harpole, Ming Sound Tsao, David Beer, Mark Watson, Frances Shepherd, William G Richards, Karla Ballman, Xiaofei Wang, zhengming Chen, Ramaswamy Govindan, guoan Chen, christopher Rivard, Fred R. Hirsch
- Abstract
- Presentation
Background
Squamous Lung Cancer (SC) which constitutes 30% of all non-small cell lung cancers (NSCLC) has few targeted therapy options for advanced disease. Surgery for early SC is the best treatment strategy; however, even patients who undergo surgery for stage IA or IB disease are still at a substantial risk for recurrence and death. Adjuvant therapy is not currently indicated for stage I SC smaller than 4 cm. Prior reports suggest gene expression-based signatures that may predict recurrence in patients with stage I SC, but none has been validated or is in clinical use. The SPECS2 Lung Cancer Consortium was assembled to compare and attempt to validate previously published prognostic signature(s) according to the guidelines proposed by Subramanian and Simon (J Natl Cancer Inst 2010; 7:327).
Method
The multi-institutional team assembled 249 frozen SC samples representing six participating institutions (cohort 1). These samples were fully annotated in a redcap database hosted by the independent statistical core. Cohort 2 was assembled utilizing 234 frozen SC samples from a prospective multi-institutional NCTN lung biobanking protocol (NCT00899782). RNA was extracted and profiled with U133A microarrays (Affymetrix) in independent core facilities. The data was transferred directly to the SPECS2 Lung statistical core in collaboration with the Alliance Statistical core and the performance of 6 most promising candidate signatures was evaluated relative to a base model that included only age, gender and AJCC stage (editions 6, 7, 8).
Result
Analysis of Cohort 1 demonstrated that only one signature (Raponi et al, Cancer Res 2006; 66:7466) significantly enhanced prognosis relative to the base model, independent of AJCC edition. This was also observed in Cohort 2, where Uno’s C index associated with AJCC 8th edition stage, sex and age (0.561; 0.468-0.654) was significantly (p <0.05) increased when the prognostic signature was added to the model (0.683; 0.611-0.755).
Conclusion
The SPECS2 Lung Cancer Consortium was successful in validating a previously published prognostic molecular signature for early stage SC using rigorous experimental design. To our knowledge, this is the first unbiased validation of a lung cancer prognostic signature using multi-institutional prospective specimens. These results support a clinical trial designed to evaluate the potential role of adjuvant therapy in completely resected early stage SC.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA13.02 - Video-Assisted Thoracoscopic Surgery vs. Thoracotomy for Non-Small Cell Lung Cancer: Survival Outcome of a Randomized Trial (Now Available) (ID 1444)
11:30 - 13:00 | Presenting Author(s): Dongrong Situ | Author(s): Hao Long, Qunyou Tan, Qingquan Luo, Zheng Wang, Gening Jiang, Tie-Hua Rong
- Abstract
- Presentation
Background
Video-assisted thoracoscopic surgery (VATS) has been widely used in the treatment of early-stage non–small cell lung cancer (NSCLC). However, there has not been a robust randomized control trial (RCT) to confirm the non-inferiority of VATS to open lobectomy in term of oncologic efficacy. Therefore, a large multicenter RCT in China was designed and initiated to verify the role of VATS.
Method
A phase 3 RCT was undertaken at five thoracic surgery tertiary centers in China. Patients aged 18-75 years old who were diagnosed of clinically early-stage NSCLCs were randomized in a 1:1 ratio into VATS and thoracotomy groups. Radical lobectomy plus hilar and mediastinal lymph node dissection was the standard surgical intervention. The primary end-point of study was 5-year overall survival (OS). The secondary end-points including 5-year disease-free survival (DFS) and cancer relapse rates would also be reported here. Analysis was by intention to treat. This study is registered with the ClinicalTrials.gov, number NCT01102517.
Result
A total of 508 patients were recruited between January 2008 and March 2014. The final follow-up for 5-year survival analysis was completed in March 2019. And 432 patients were eligible for analysis (222 cases in VATS group and 210 cases in thoracotomy group). The cancer relapse (recurrence and metastasis) rates were 39.2% in VATS group and 36.7% in thoracotomy group respectively (P=0.621). Patients who received VATS lobectomies had a similar 5-year DFS to those who underwent open surgery (58% versus 62%, P=0.686). Finally, the 5-year OS rates were of no significant difference between VATS and thoracotomy groups (74% versus 71%, P=0.497).
Conclusion
The non-inferiority of VATS to thoracotomy lobectomy was confirmed in our RCT in terms of oncologic efficacy for clinically early-stage NSCLCs.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA13.03 - Predicting Postoperative Recurrence in Completely Resected EGFR-Mutant Non-Small Cell Lung Cancer: Value of IHC Markers (Now Available) (ID 998)
11:30 - 13:00 | Presenting Author(s): Zhengfei Zhu | Author(s): tiantian Guo, Jianjiao Ni, Yuan Li
- Abstract
- Presentation
Background
EGFR mutations are detected in up to 50% of non-small cell lung cancer (NSCLC) and recent studies indicate that EGFR-mutant NSCLC is a heterogeneous disease with varying co-mutations, diverse histologic subtypes and distinct expression of oncoproteins. However, the risk factors and clinical patterns of postoperative recurrence among patients with completely resected EGFR-mutant NSCLC have not been fully understood. Moreover, the prognostic values of routinely used immunohistochemical (IHC) markers in NSCLC are seldom reported.
Method
Consecutive patients with curative resected NSCLC and confirmed EGFR mutations at Fudan University Shanghai Cancer Center from January 2007 to December 2017, were retrospectively enrolled. The initial recurrence sites were recorded and categorized into five groups: thoracic recurrence, brain recurrence, neck recurrence, abdominal recurrence, and bone recurrence. The indicators of overall and site-specific recurrence were identified using the Cox regression model, where a panel of routinely used IHC markers (including Her2, Ki67, TTF-1, CK20, CK7, CK5/6, p53, RRM1, NapsinA, p40, syn, Bcl-2, CDX2, ERCC1 and p63) were incorporated. A nomogram was developed based on variables selected in multivariate analysis. The bootstrapping method (1000 repetitions) was applied to internally validate the nomogram
Result
After a median follow-up of 32 (range, 5-122) months, disease recurrence was observed in 197(37.1%) out of the 531 patients, with a median recurrence-free survival (RFS) of 19 (95% CI, 16.63-21.37) months. Most patients (n=136; 69.0%) had thoracic recurrence, followed by brain recurrence (n=41; 20.8%), bone recurrence (n=41; 20.8%), abdominal recurrence (n=14; 7.1%), and neck recurrence (n=13; 6.6%). Sex, tumor size, Ki67, and N stage were independent indicators of thoracic recurrence. Tumor size, N stage, CK20, and Syn were independent indicators of brain recurrence. N stage and Ki67 were independent indicators of bone recurrence. N stage was the independent indicator of abdominal recurrence and neck recurrence. Tumor size, Ki67, CK20, and N stage were independently associated with overall recurrence, and thus a nomogram predicting the 1-, 2-, and 3-year RFS probability was developed based on these four factors. The concordance index (C-index) was 0.723 (95% confidence interval, 0.675 to 0.771) and the calibration curves displayed good agreement between the predicted RFS and the actual observation.
Conclusion
Independent prognostic indicators based on clinic-pathological parameters and routinely used IHC markers were identified to predict overall and site-specific recurrence, which may help to identify optimal candidates for adjuvant therapies and design individualized surveillance strategies among patients with completely resected EGFR-positive NSCLC
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA13.04 - Discussant - OA13.01, OA13.02, OA13.03 (Now Available) (ID 3794)
11:30 - 13:00 | Presenting Author(s): Kemp Kernstine
- Abstract
- Presentation
Abstract not provided
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA13.05 - NADIM Study: Updated Clinical Research and Outcomes (Now Available) (ID 1670)
11:30 - 13:00 | Presenting Author(s): Mariano Provencio | Author(s): Ernest Nadal, Amelia Insa, Rosario Garcia Campelo, JOAQUIN Casal, Manuel Dómine, Margarita Majem, Delvys Rodriguez-Abreu, Alex Martinez-Marti, Javier De Castro Carpeno, Manuel Cobo, Guillermo López-Vivanco, Elvira Del Barco, Reyes Bernabe, Nuria Viñolas, Isidoro Barneto, Santiago Viteri, Paloma Martin Martorell, Maria Jove, Virginia Calvo De Juan, Bartomeu Massuti
- Abstract
- Presentation
Background
Patients with stage IIIA (N2 or T4N0) are potentially curable but median overall survival is only around 15 months
Method
A Phase II, single-arm, open-label multicenter study of resectable stage IIIA N2-NSCLC in adult patients with CT plus IO as neoadjuvant treatment: 3 cycles of nivolumab (NV) 360 mg IV Q3W + paclitaxel 200 mg/m2 + carboplatin AUC 6 IV Q3W followed by adjuvant NV treatment for 1 year. After completing neoadjuvant therapy, all patients underwent tumor assessment prior to surgery. Surgery was performed during the 3rd or 4th week after day 21 of the 3rd neoadjuvant treatment cycle. The study aimed to recruit 46 patients. The primary endpoint was Progression-Free Survival (PFS) at 24 months. Efficacy was explored using objective pathologic response criteria. Here we present the final data on all study patients that underwent surgical assessment.
Result
At the time of submission, the 46 patients had been included. None of the patients were withdrawn from the study preoperatively due to progression or toxicity. 41 patients had undergone surgery and all tumors were deemed resectable with R0 resection in all cases. Intention to treat analysis shows 35 patients (85%; 95% CI, 71; 94%) achieved major pathologic response (MPR) of which 25 (71%; 95% CI, 54; 85%) were complete pathologic responses (CPR). Downstaging was seen in 38 (93%; 95% CI, 80; 98%) of cases. The median follow-up was 13.8 months (P25; P75: 11.7; 16.6 months) for both the whole series and resected patients, and 12 month PFS was 95.7% (95% CI, 84; 99%).
Conclusion
This is the first multicentric study to test CT-IO in the neoadjuvant setting in stage IIIA. Neoadjuvant CT-IO with nivolumab in resectable IIIA NSCLC yields a complete pathologic response rate that is higher than ever seen previously, together with a promising PFS which may translate into increased overall survival. EudraCT Number: 2016-003732-20. Clinical trial information: NCT 03081689.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA13.06 - Surgical Outcomes Following Neoadjuvant Nivolumab or Nivolumab Plus Ipilimumab in Non-Small Cell Lung Cancer - NEOSTAR Study (Now Available) (ID 2041)
11:30 - 13:00 | Presenting Author(s): Boris Sepesi | Author(s): Tina Cascone, William N. William, Heather Lin, Cheuk Leung, Annikka Weissferdt, Garrett L Walsh, David Rice, Jack Roth, Reza J Mehran, Wayne L Hofstetter, Mara Antonoff, Frank Fossella, Frank E Mott, Xiuning Le, Ferdinandos Skoulidis, Jianjun Zhang, Lauren Averett Byers, Vincent Lam, Bonnie Glisson, Jonathan Kurie, George Blumenschein, Anne Tsao, Charles Lu, Mehmet Altan, Yasir Elamin, Don Lynn Gibbons, Vassiliki A Papadimitrakopoulou, Jack Lee, John Victor Heymach, Ara A Vaporciyan, Stephen Swisher
- Abstract
- Presentation
Background
Surgical outcomes following neoadjuvant immune checkpoint inhibitors (ICIs) are limited. We report 90-day perioperative results of the NEOSTAR phase II trial of neoadjuvant nivolumab or nivolumab/ipilimumab in resectable non-small cell lung cancers (NSCLCs).
Method
44 pts with stage I-IIIA NSCLC (AJCC 7th) were randomized to nivolumab (3 mg/kg IV, days 1, 15, 29, n=23) or nivolumab/ipilimumab (1 mg/kg IV, day 1, n=21) with resection planned between 3-6 weeks after last dose. Surgical approach and extent of resection were at surgeons’ discretion.
Result
39 (89%) patients underwent R0 resection, of those 2 (5%) were resected off trial after additional induction chemotherapy (1 nivolumab, 1 nivolumab/ipilimumab). Among 37 patients, 21 underwent surgery following nivolumab and 16 following nivolumab/ipilimumab. Median age 66 (43-83) years, 24 (65%) male, 33 (89%) white, 22 (59%) adenocarcinoma, 22 (59%) stage I, 9 (24%) stage II, 6 (16%) stage IIIA.
5 (11%) were not resected, 1 (1/23, 4%) after nivolumab (stage II), 4 (4/21, 19%) after nivolumab/ipilimumab (1 stage I, 1 stage II, 2 stage IIIA). Reasons for unresectability were change in surgeon’s judgement (n=2), toxicity (n=1), progression (n=1), and declining pneumonectomy (n=1). Median time to surgery was 31 days (range 21-87). 8 (22%) operations were delayed beyond 42 days, 5 after nivolumab/ipilimumab (5/16, 31%) and 3 after nivolumab (3/21, 14%).
33 (89%) underwent lobectomy, 2 (5%) pneumonectomy, 1 (3%) segmentectomy and 1 (3%) wedge resection. 27 (73%) had thoracotomy, 7 (19%) thoracoscopy, 3 (8%) robotic approach. 2 (5%) were electively converted from thoracoscopy to thoracotomy. Median operative time was 147 minutes (71-315), median blood loss was 100cc (50-1000), and median length of stay was 4 days (1-18).
Perioperatively, pulmonary complications occurred in 8 (22%) patients: 8 (22%) prolonged air leak, 2 (5%) pneumonitis/pneumonias, 1 (3%) empyema, and 1 (3%) bronchopleural fistula (BPF). 1 (3%) died from complications of BPF and steroid therapy for pneumonitis. 4 (11%) developed atrial fibrillation, 1 (3%) diarrhea, 1 (3%) ileus, and 1 (3%) transient ischemic attack.
Surgeons subjectively judged 15/37 (40%) of operations to be more complex than usual with 7/37 (19%) lasting > 4 hours.
Conclusion
Following three cycles of neoadjuvant ICIs 89% of patients underwent complete R0 resection, including two patients who received additional induction chemotherapy off trial. Five marginally operable patients who didn’t proceed to resection, and one perioperative mortality highlight the importance of cautious patient selection for neoadjuvant ICIs in the management of operable NSCLC.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA13.07 - Neoadjuvant Atezolizumab in Resectable NSCLC Patients: Immunophenotyping Results from the Interim Analysis of the Multicenter Trial LCMC3 (Now Available) (ID 1755)
11:30 - 13:00 | Presenting Author(s): Filiz Oezkan | Author(s): Kai He, Dwight Hall Owen, Maciej Pietrzak, Ju Hwan Cho, Rhonda Kitzler, Rebecca Pearson, Valerie W. Rusch, Jamie E. Chaft, Robert Suh, Justin D Blasberg, Karen L Reckamp, Dan J Raz, Peter J Kneuertz, Lauren Fiorillo, Edward Garon, Alan Nicholas, Ann Johnson, Katja Schulze, Jessica Grindheim, Romain Banchereau, See-Chun Phan, Paul A Bunn, Jr, David J Kwiatkowski, Bruce E Johnson, Mark G Kris, Ignacio Wistuba, Jay M Lee, Gerard Lozanski, David P Carbone
- Abstract
- Presentation
Background
The immune mechanisms dictating response and resistance to PD-(L)1 blockade are not well understood in early stage non-small cell lung cancer (NSCLC). Understanding these mechanisms will be key to improve outcomes and identify the next generation of predictive biomarkers of response to these therapies. Here, we present updated immunophenotyping at time of interim analysis of LCMC3, a multicenter trial of neoadjuvant atezolizumab in resectable NSCLC (NCT02927301).
Method
Patients received 2 cycles of atezolizumab before resection. Tumor, LN biopsies and PB were obtained pre-atezolizumab and at surgery. Paired PB, screening and surgical LN were analyzed using IMMUNOME flow cytometry. Plasma-based cytokine arrays were performed on a subset of patients. Immunophenotypic analyses were correlated with treatment effect, major pathologic response (MPR, primary endpoint) and preoperative treatment-related adverse events (preop-TRAE).
Result
We report on 55 patients with paired PB samples (analyzed within 72h after collection) and completed surgery. We observed preop-TRAE in 32/55 patients (18 grade 1, 13 grade 2, 1 grade 3). CD1c+ and CD141+ myeloid cells (MC) were lower at baseline in patients developing preop-TRAEs, while monocytic M-MDSCs were higher in those patients. Senescent T cells decreased in patients with preop-TRAE and increased in patients with non-preop-TRAE. After treatment, the absolute cell counts of late activated CD4+and CD8+T cells decreased in patients achieving MPR. LN IMMUNOME data, cytokine data and 12-month follow-up (DFS, OS) will be reported.
Conclusion
Preliminary immunophenotyping data from the interim analysis showed significantly lower baseline immunosuppressive cell subsets in patients with preop-TRAE and decreased late activated CD4+and CD8+T cells from PB in patients with MPR.These results, together with additional LN IMMUNOME and cytokine analyses, may improve our understanding of immunophenotypic features associated with outcome, and changes induced by neoadjuvant atezolizumab in early stage NSCLC patients.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA13.08 - Discussant - OA13.05, OA13.06, OA13.07 (Now Available) (ID 3795)
11:30 - 13:00 | Presenting Author(s): Harvey I Pass
- Abstract
- Presentation
Abstract not provided
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA13.09 - Robert J. Ginsberg Lectureship Award for Surgery (Now Available) (ID 3899)
11:30 - 13:00 | Presenting Author(s): Giulia Veronesi
- Abstract
- Presentation
Abstract not provided
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.


