Virtual Library
Start Your Search
Humberto Choi
Author of
-
+
P2.17 - Treatment of Early Stage/Localized Disease (ID 189)
- Event: WCLC 2019
- Type: Poster Viewing in the Exhibit Hall
- Track: Treatment of Early Stage/Localized Disease
- Presentations: 1
- Moderators:
- Coordinates: 9/09/2019, 10:15 - 18:15, Exhibit Hall
-
+
P2.17-34 - Integrated Clinico-Radiomic Nomogram for Predicting Disease-Free Survival (DFS) in Stage I and II Non-Small Cell Lung Cancer (ID 2886)
10:15 - 18:15 | Author(s): Humberto Choi
- Abstract
Background
Early stage non-small cell lung cancer (ES-NSCLC) comprises about 45% of all NSCLC patients, with 5-year survival ranging between 30-49%. Surgical resection is the standard of care curative modality in these patients but about 30-55% of patients often recur following surgery within the first 3 years. There is currently no validated method to stratify patients based on their risk of recurrence following surgery in these patients. In this project, we develop and validate a nomogram using a combination of CT-derived radiomic textural features and clinco-pathologic factors, in order to predict DFS in ES-NSCLC.
Method
This study comprised 350 ES-NSCLC patients from two different institutions who underwent surgery (75 patients relapsed). Radiomic textural features were extracted from tumor region (Intratumoral - IT) as well as from the annular ring shaped peritumoral region (PT) with 3mm as a ring thickness and extending 9 mm outside the nodule. A total of 124 features from Gabor, Laws, Laplace, Haralick and Collage feature families were extracted from IT and each PT ring for all patients. The most stable, significant and uncorrelated features were selected from D1 (N=221) and used to build a Lasso-regularized multivariate Cox-regression model to generate a Radiomic Risk Score (RRS) derived from weighted Lasso coefficients. Further, RRS was integrated with clinic-pathologic variables (Lympho-vascular invasion LVI and AJCC stage) which were independently predictive on DFS in multivariate analysis to build a clinical-radiomics score (CRS). A nomogram was constructed to visually assess the CRS and RRS on DFS. Performances were evaluated using hazard ratios (HR), concordance index (C-Index) along with decision and calibration curves to show the differences between the individual and integrated risk scores.
Result
Top 14 radiomic features included 6 from IT and 8 from 0-9 mm PT distance. The constructed RRS could predict DFS (n=221, C-index=0.69, HR = 3.8; 95% CI- 2.7-5.6, p<0.05) on training (D1) and (n=129, C-index=0.69, HR – 2.5; 95% CI – 1.8-4.7; p<0.05) on a blinded validation cohort (D2), Addition of LVI and pN to build the CRS, increased C-index to 0.74, (p<0.05). Decision and calibration curve analysis shows improved performance of CRS over RRS or clinco-pathologic factors alone.
Conclusion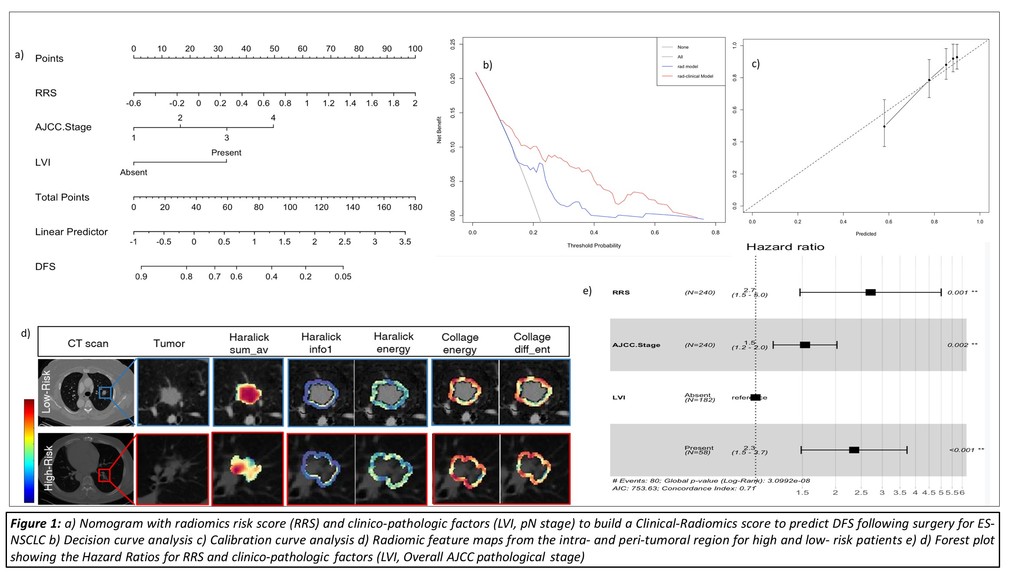
Addition of prognostic clinical factors (LVI, AJCC stage) improved the performance of the Radiomic Risk Score model in order to accurately predict DFS in ES-NSCLC patients undergoing surgery.


