Virtual Library
Start Your Search
Amit Gupta
Author of
-
+
P2.04 - Immuno-oncology (ID 167)
- Event: WCLC 2019
- Type: Poster Viewing in the Exhibit Hall
- Track: Immuno-oncology
- Presentations: 1
- Moderators:
- Coordinates: 9/09/2019, 10:15 - 18:15, Exhibit Hall
-
+
P2.04-16 - Novel CT Based Radiomic Features are Prognostic and Predictive of Benefit of Chemoimmunotherapy in Advanced Non-Squamous NSCLC (ID 2769)
10:15 - 18:15 | Author(s): Amit Gupta
- Abstract
Background
Carboplatin, pemetrexed and pembrolizumab (C/P/P) is currently approved for patients with advanced non-squamous carcinoma of the lung (NS-NSCLC) based on superior survival outcomes noted in KEYNOTE-189. Since clinical benefit was observed across all PD-L1 expression categories, there are currently no robust predictive biomarkers that can identify subsets of patients likely to derive benefit from this regimen. We sought to evaluate whether radiomic features extracted from within and outside the nodule on pre-therapy CT scans could predict response to C/P/P.
Method
We retrospectively identified 52 patients with stage IV NS-NSCLC who received C/P/P. Of these, 6 were excluded because of non-evaluable thoracic lesions. Lung tumors were contoured on 3D SLICER software by an expert reader. Textural and shape radiomic features were extracted from intra/peritumoral regions using MATLAB® 2018b platform (Mathworks, Natick, MA). The primary endpoint of our study was RECIST response and secondary end point was overall survival (OS). A linear discriminant analysis classifier (LDA) was used to predict response across 100 iterations of threefold cross validation in the dataset. Performance of classifier on response was measured by area under receiver operating characteristic curve (AUC). To build the multivariate radiomic signature for OS, least absolute shrinkage and selection operator (LASSO) Cox regression model was used and a risk score was computed according to a linear combination of selected features. Patients were divided into high-risk or low-risk groups based on median risk score.
Result
The top five radiomic features (intra/peritumoral textural patterns) predictive of response to C/P/P were identified by mRMR feature selection method. LDA classifier using these features could discriminate responders from non-responders with an AUC of 0.77 ± 0.05.
The radiomic risk score was calculated using a linear combination of top six selected features from LASSO with corresponding coefficients. In a multivariate Cox proportional hazards model using a combination of clinicopathologic and radiomic features, the radiomics signature was found to be significantly associated with OS (averaged on 100 iteration of CV) (HR 10.42; 95% CI: 4.18-26; P = 4.92e-07). Kaplan-Meier survival analyses according to the radiomics signature risk-score showed significantly worse survival in the high risk category.
Conclusion
Textural features within and outside the nodule on pre-treatment CT images of patients with NS-NSCLC treated with C/P/P were predictive of responses and OS. Additional validation of these quantitative image-based biomarkers in independent cohorts is warranted.
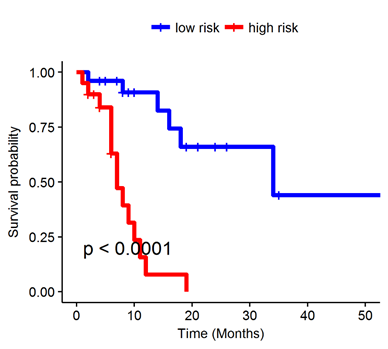
Figure: Kaplan-Meier survival analyses of patients (N = 46) with NS-NSCLC treated with C/P/P using the radiomics signature risk-score.
-
+
P2.17 - Treatment of Early Stage/Localized Disease (ID 189)
- Event: WCLC 2019
- Type: Poster Viewing in the Exhibit Hall
- Track: Treatment of Early Stage/Localized Disease
- Presentations: 1
- Moderators:
- Coordinates: 9/09/2019, 10:15 - 18:15, Exhibit Hall
-
+
P2.17-34 - Integrated Clinico-Radiomic Nomogram for Predicting Disease-Free Survival (DFS) in Stage I and II Non-Small Cell Lung Cancer (ID 2886)
10:15 - 18:15 | Author(s): Amit Gupta
- Abstract
Background
Early stage non-small cell lung cancer (ES-NSCLC) comprises about 45% of all NSCLC patients, with 5-year survival ranging between 30-49%. Surgical resection is the standard of care curative modality in these patients but about 30-55% of patients often recur following surgery within the first 3 years. There is currently no validated method to stratify patients based on their risk of recurrence following surgery in these patients. In this project, we develop and validate a nomogram using a combination of CT-derived radiomic textural features and clinco-pathologic factors, in order to predict DFS in ES-NSCLC.
Method
This study comprised 350 ES-NSCLC patients from two different institutions who underwent surgery (75 patients relapsed). Radiomic textural features were extracted from tumor region (Intratumoral - IT) as well as from the annular ring shaped peritumoral region (PT) with 3mm as a ring thickness and extending 9 mm outside the nodule. A total of 124 features from Gabor, Laws, Laplace, Haralick and Collage feature families were extracted from IT and each PT ring for all patients. The most stable, significant and uncorrelated features were selected from D1 (N=221) and used to build a Lasso-regularized multivariate Cox-regression model to generate a Radiomic Risk Score (RRS) derived from weighted Lasso coefficients. Further, RRS was integrated with clinic-pathologic variables (Lympho-vascular invasion LVI and AJCC stage) which were independently predictive on DFS in multivariate analysis to build a clinical-radiomics score (CRS). A nomogram was constructed to visually assess the CRS and RRS on DFS. Performances were evaluated using hazard ratios (HR), concordance index (C-Index) along with decision and calibration curves to show the differences between the individual and integrated risk scores.
Result
Top 14 radiomic features included 6 from IT and 8 from 0-9 mm PT distance. The constructed RRS could predict DFS (n=221, C-index=0.69, HR = 3.8; 95% CI- 2.7-5.6, p<0.05) on training (D1) and (n=129, C-index=0.69, HR – 2.5; 95% CI – 1.8-4.7; p<0.05) on a blinded validation cohort (D2), Addition of LVI and pN to build the CRS, increased C-index to 0.74, (p<0.05). Decision and calibration curve analysis shows improved performance of CRS over RRS or clinco-pathologic factors alone.
Conclusion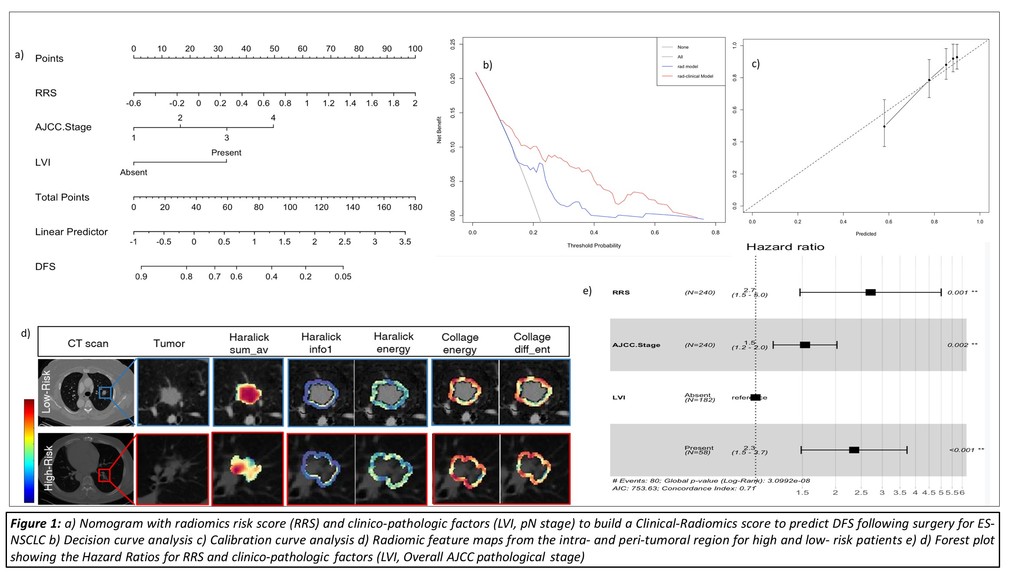
Addition of prognostic clinical factors (LVI, AJCC stage) improved the performance of the Radiomic Risk Score model in order to accurately predict DFS in ES-NSCLC patients undergoing surgery.


