Virtual Library
Start Your Search
Jalen A Benson
Author of
-
+
OA08 - Advanced Models and "Omics" for Therapeutic Development (ID 133)
- Event: WCLC 2019
- Type: Oral Session
- Track: Biology
- Presentations: 1
- Now Available
- Moderators:Luis M Montuenga, Julie George
- Coordinates: 9/09/2019, 11:00 - 12:30, Interlaken (1988)
-
+
OA08.03 - A Single-Cell Resolution Map of EMT and Drug Resistance States for Evaluating NSCLC Clinical Specimens (Now Available) (ID 2771)
11:00 - 12:30 | Author(s): Jalen A Benson
- Abstract
- Presentation
Background
The role of epithelial-mesenchymal transition (EMT) in NSCLC is well reported and has been shown to prime cells for metastasis. EMT can be adopted or reversed (i.e. mesenchymal-epithelial transition, MET) by cells, revealing plasticity that can also lead to drug resistance. Although it is appreciated that EMT is not a binary process of two extremes but instead a spectrum of intermediate states of EMT phenotypes, these are poorly defined at the single-cell proteomic level in NSCLC clinical specimens. Our overall goal was to dynamically capture and characterize EMT-related drug resistance states in lung cancer cells to construct a single-cell resolution state map of clinical applicability.
Method
We used mass cytometry (CyTOF) time-course experimentation and novel computational tools to analyze TGFβ and drug treated NSCLC cell lines, as well as NSCLC clinical samples to identify clinically relevant drug resistant EMT and MET states and construct a single-cell resolution proteomic map of phenotypic states.
Result
Through TGFβ treatment and withdrawal we resolved previously unrealized EMT and MET states in NSCLC cell lines by analyzing the expression of up to 30 surface and intracellular markers. Using a novel computational tool (TRACER) we also provide evidence that EMT and MET trajectories differ and exert differential drug sensitivity profiles. We used the identified EMT and MET states to construct a NSCLC reference EMT-MET state map, on which we projected NSCLC clinical samples to characterize their phenotypic profile in terms of our in vitro EMT-MET analysis. Finally, we extended our mass cytometry time-course analysis to NSCLC cells that underwent various drug treatments (e.g. Erlotinib, Docetaxel) and subsequent withdrawal to augment our EMT-MET state map with drug resistance phenotypic traits. We found that NSCLC resistant cells displayed through time overlapping morphological and cell signaling features with EMT and MET and were able to rebound from short-term drug-induced effects. These data are currently being used to evaluate EMT-related drug resistant cell states detected in pleural effusions during and after the course of treatment in different NSCLC patient therapy time-points.
Conclusion
In summary, we provide a framework that can be extended to phenotypically characterize clinical samples with single-cell resolution in the context of in vitro studies showing differential EMT-MET traits related to drug sensitivity. This sets the foundation for developing tools towards evaluating - at a personalized level – disease status and response to treatment in NSCLC patients.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
P2.05 - Interventional Diagnostic/Pulmonology (ID 168)
- Event: WCLC 2019
- Type: Poster Viewing in the Exhibit Hall
- Track: Interventional Diagnostics/Pulmonology
- Presentations: 1
- Moderators:
- Coordinates: 9/09/2019, 10:15 - 18:15, Exhibit Hall
-
+
P2.05-01 - Broad Genomic Profiling of Bronchoalveolar Lavage Fluid in Lung Cancer (ID 615)
10:15 - 18:15 | Author(s): Jalen A Benson
- Abstract
Background
We hypothesized that tumor-derived mutations from non-small cell lung cancer (NSCLC) are readily detectable in bronchoalveolar lavage (BAL). To explore our hypothesis, we employed the CAncer Personalized Profiling by deep Sequencing (CAPP-Seq) method to identify somatic mutations in BAL compared to blood.
Method
We profiled 200 matching lavage, plasma, and PBMC samples from a total of 38 NSCLC patients and 21 controls. We first applied a tumor-informed calling approach to most sensitively detect mutations in BAL and plasma. We then applied a tumor-naïve mutation calling strategy to explore the effect of field cancerization in at risk patients with lung nodules or who smoked. Last, we developed a BAL mutation classifier to differentiate patients with cancer from those without and compared the performance of this classifier to BAL cytology.
Result
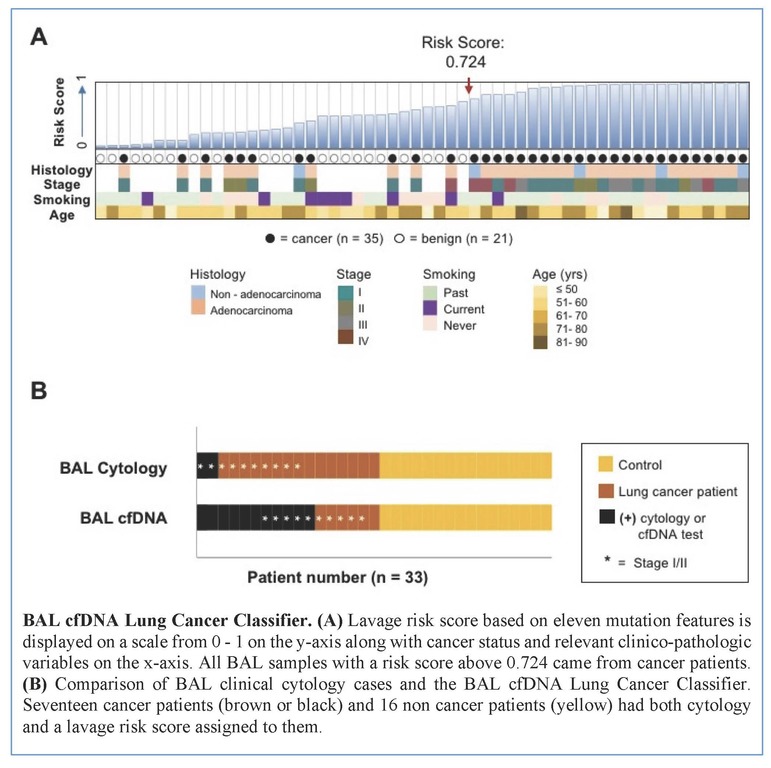
Tumors were primarily lung adenocarcinomas (84%) and mostly early stage disease (I-II 71%; III-IV 29%). We called a median of 4 mutations per tumor. TP53 and KRAS were the most frequently detected variants in tumor (47% and 35% respectively) and lavage cell free (cf) DNA (38% and 26% respectively). Using a tumor-informed approach, we detected significantly more variants in lavage cfDNA than in plasma from cancer patients (p<0.001) and variants were more frequently called in lavage cfDNA than in plasma from cancer patients (77% vs. 41%, p=0.004). As expected, tumor-naïve calling resulted in fewer variants detected in both sample types when compared to tumor-informed calling but we identified more tumor mutations (p<0.001) and more putative cancer driver mutations (p< 0.003) in lavage cfDNA than in plasma. Mutations of cancer driver genes at the patient level and average %VAF at the gene level were significantly lower in lavage cfDNA controls compared to cancer patients (p=0.017 and p=0.016 respectively). Since we also detected mutations in controls, presumably secondary to field cancerization and somatic mosaicism, we developed a risk score of mutation features to classify whether a BAL specimen was likely to come from a cancer patient or control. At a risk score level that identified all non-cancers as benign (A), this BAL classifier of 11 mutation features identified more cancers than cytology for all stages of lung cancer (65% vs 12%, p=0.001) and in stage I/II disease (50% vs. 20%, p=0.25; B).
Conclusion
We show here that BAL genomic profiling may augment plasma profiling and BAL cytology for diagnosing and profiling NSCLC. Validation studies will be required to confirm our findings.


