Virtual Library
Start Your Search
Shun-ichi Watanabe
Author of
-
+
EP1.18 - Treatment of Locoregional Disease - NSCLC (ID 208)
- Event: WCLC 2019
- Type: E-Poster Viewing in the Exhibit Hall
- Track: Treatment of Locoregional Disease - NSCLC
- Presentations: 1
- Now Available
- Moderators:
- Coordinates: 9/08/2019, 08:00 - 18:00, Exhibit Hall
-
+
EP1.18-03 - Outcome of Surgical Resection for Invasive Mucinous Adenocarcinoma: Experience at a Single Institution (Now Available) (ID 2105)
08:00 - 18:00 | Author(s): Shun-ichi Watanabe
- Abstract
Background
Invasive mucinous adenocarcinomas are new histological type which was determined by WHO classification 4thedition. The aim of this study was to investigate the outcome of surgical treatment for the patients with invasive mucinous adenocarcinoma who underwent surgery in our institution.
Method
Between 2010 and 2013, We identified 68 patients with invasive mucinous adenocarcinoma who underwent surgical resection. We measured the distance of tumor cell size and mucinous size, and their clinical and pathological data were retrospectively reviewed. Overall survival (OS) rates were compared using a log-rank test and survival curves were plotted using the Kaplan–Meier method.
Result
Participants comprised 31 men and 37 women, ranging in age from 46 to 83 years (median, 67 years). Median observation period in the survivors was 5.1 years. T classification of group oftumor cell size was T1/T2/T3,4=42/17/9 cases, and group of mucinous size was T1/T2/T3,4=38/17/13 cases. The 5-year overall survival rate for group oftumor cell sizewere T1/T2/T3,4=94.3/88.3/60.5%, and group of mucinous size were MS:T1/T2/T3,4=94.1/85.7/70.0%(5Y-OS tumor cell size / mucinous size : p=0.02/p=0.147, 5Y-RFS tumor cell size / mucinous size : p=0.04/p=0.237).
Conclusion
Our result indicated that to determine T classification, we should measure the distance of tumor cell size instead of mucinous size.
-
+
MA06 - Challenges in the Treatment of Early Stage NSCLC (ID 124)
- Event: WCLC 2019
- Type: Mini Oral Session
- Track: Treatment of Early Stage/Localized Disease
- Presentations: 1
- Now Available
- Moderators:Florentino Hernando-Trancho, Ayten Kayi Cangir
- Coordinates: 9/08/2019, 13:30 - 15:00, Colorado Springs (1994)
-
+
MA06.06 - A Phase III Study of Adjuvant Chemotherapy in Patients with Completely Resected, Node-Negative Non-Small Cell Lung Cancer (Now Available) (ID 285)
13:30 - 15:00 | Author(s): Shun-ichi Watanabe
- Abstract
- Presentation
Background
Post-operative UFT (tegafur/uracil) has been shown to prolong survival of Japanese patients with completely resected, p-stage I (T1> 2 cm) non-small cell lung cancer (NSCLC). This trial, the Japan Clinical Oncology Group (JCOG) 0707, aimed at estimating the efficacy of S-1 (tegafur/gimeracil/oteracil) compared to UFT as adjuvant therapy in this population.
Method
Eligible patients had received complete resection with lymph node dissection for p-stage I (T1-2N0M0, T1> 2 cm, by 5thEdition UICC TNM) NSCLC, within 56 days of enrollment. Patients were randomized to receive: oral UFT 250mg/m2/day for 2 years (Arm A), or oral S-1 80mg/m2/day for 2 weeks and 1 week rest, for 1 year (Arm B). The initial primary endpoint was overall survival (OS). Based upon the monitoring in Jun. 2013, which showed the combined OS of the 2 arms better than expected (4-year OS of 91.6% vs. presumed 5-year OS of 70-76.5%), it was judged to be underpowered. The study protocol was amended so that the primary endpoint is relapse-free survival (RFS). With the calculated sample size of 960, this study would detect the superiority of Arm B over Arm A with power 80% and one-sided type I error of 0.05, assuming the 5-year RFS of 75% in Arm A and the hazard ratio of 0.75.
Result
From Nov. 2008 to Dec. 2013, 963 patients were enrolled (Arm A : 482, Arm B : 481): median age 66 (range: 33 to 80), male 58%, adenocarcinoma 80%, p-T1/T2 46%/54%. Only 2 received pneumonectomy. >Grade 3 toxicities (hematologic/nonhematologic) were observed in 15.9 (1.5/14.7) % in Arm A, and in 14.9 (3.6/12.1) % in Arm B, respectively. 60.0% of the patients in Arm A and 54.7% of them in Arm B completed the protocol treatment (p=0.10). There were 4 cases of deaths during protocol treatment, probably of cardio-vascular origin, with 1 in Arm A and 3 in Arm B. At the data cut-off of Dec. 2018, the hazard ratio (HR, Arm B vs. Arm A) of RFS was 1.06 (95% confidence interval (C.I.): 0.82-1.36), showing no superiority of S-1 over UFT. The HR of OS was 1.10 (95% C.I.: 0.81-1.50). The 5-year RFS/OS rates were 79.4%/88.8% in Arm A and 79.5%/89.7% in Arm B, respectively. Pre-specified subset analyses for gender, age, smoking, stage, tumor side, lymph node dissection area, pleural invasion and histology revealed no remarkable results; S-1 arm was not superior to UFT arm in each analysis. Of the 77 and 85 OS events for Arm A/Arm B, 45 each (58%/53%, respectively) were due to the NSCLC. During the follow-up period, secondary malignancy was observed in 85 (17.8%) and 84 (17.8%) in Arm A and Arm B, respectively.
Conclusion
Post-operative adjuvant therapy with oral S-1 was not superior to that with UFT in stage I (T>2 cm) NSCLC after complete resection. UFT remains standard in this population. Future investigation should incorporate identification of high-risk population for recurrence, since survival of each arm was so good with substantial number of OS events due to other causes of deaths in this trial.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
MA08 - Pawing the Way to Improve Outcomes in Stage III NSCLC (ID 127)
- Event: WCLC 2019
- Type: Mini Oral Session
- Track: Treatment of Locoregional Disease - NSCLC
- Presentations: 1
- Now Available
- Moderators:Simon Ekman, Helena A Yu
- Coordinates: 9/08/2019, 15:15 - 16:45, Tokyo (1982)
-
+
MA08.06 - Perioperative Outcomes of Lung Cancer Patients with Interstitial Pneumonia (Now Available) (ID 1372)
15:15 - 16:45 | Author(s): Shun-ichi Watanabe
- Abstract
- Presentation
Background
Interstitial lung disease is mostly found in elderly male smokers who also have relatively high risks of developing lung cancer. For these patients, modality to treat malignancy is limited to prevent acute exacerbation of interstitial pneumonia. We analyzed the perioperative outcomes of this group of patients with both interstitial pneumonitis and resectable lung cancer with curative intent.
Method
We retrieved the characteristics and medical courses of consecutive patients who had undergone pulmonary resections from medical records. In this analysis, usual interstitial pneumonia (UIP) was characterized by the presence of basal predominant, subpleural reticular abnormalities with traction bronchiectasis and honeycomb cysts detected in bilateral lung field on chest computed tomography preoperatively. Pathological findings on surgical specimen were used confirmation of diagnosis. The incidence and outcomes of acute exacerbation within 30 days from operation were analysed.
Result
From 2015 to 2017, there were 1,477 patients who underwent pulmonary resection for primary lung cancer at our institute. Among them there were 81 (5.5%) patients diagnosed as UIP by specific findings on chest computed tomography. Of 81 patients evaluated, 68 (84.0 %) were men, the median age was 73 years (range, 55-88). For Eastern Cooperative Oncology Group (ECOG) performance status, all 81 patients were categorized in status 0. Seventy-four patients (91.4%) underwent lobectomy, 1 (1.2%) bi-lobectomy, 2 (2.5%) segmentectomy and 4 (4.9%) wide wedge resections for primary lung cancer. The mean duration of surgery was 129 mins (range, 54-316), and mean value for blood loss was 36.5 ml (range, 0-396). A complete resection (R0) was achieved in 79 cases (97.5%). Postoperative complications were observed in 19 patients (23.5%) including prolonged air leakage (n=4, 4.9%), late onset of air leakage (n=3, 3.7%), surgical site infection, chylothorax and cerebral infarction. Nine patients (11.1%) manifested acute exacerbation of interstitial pneumonia within 30 days after surgery. There were 3 post-operative deaths (3.7%) within 30 days after surgery. Two deaths (2.5%) were due to acute exacerbation of interstitial pneumonia and 1 (1.2%) case of SAH on 1POD.
Conclusion
Pulmonary resection for patients with interstitial lung disease led to 9 (11.1%) cases of acute exacerbation within 30 days from surgery. Mortality related to acute exacerbation was found only 2 cases (2.5%) at our hospital, which was tolerable postoperative outcome for pulmonary resection for lung cancer with curative intent.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
MA15 - Usage of Computer and Molecular Analysis in Treatment Selection and Disease Prognostication (ID 141)
- Event: WCLC 2019
- Type: Mini Oral Session
- Track: Pathology
- Presentations: 1
- Now Available
- Moderators:John Le Quesne, Noriko Motoi
- Coordinates: 9/09/2019, 15:45 - 17:15, Tokyo (1982)
-
+
MA15.03 - Exploring Digital Pathology-Based Morphological Biomarkers for a Better Patients’ Selection to the Immune Checkpoint Inhibitor of Lung Cancer (Now Available) (ID 1777)
15:45 - 17:15 | Author(s): Shun-ichi Watanabe
- Abstract
- Presentation
Background
For eligible patients’ selection for immune checkpoint inhibitor therapy (ICI), it is important to establish more accurate predicting biomarkers, in addition to PD-L1 IHC and MSI-high. We hypothesized that morphological characteristics should reflect genetic alteration, thus could predict ICI responsiveness. In this study, we examined the predictive potential of morphological characteristics using digital whole-slide images as a new biomarker for ICI-treatment on non-small cell lung cancer (NSCLC) and their relationship to PD-L1 IHC and genetic alterations.
Method
71 NSCLC who received ICI therapy were recruited. Digital images of H&E and PD-L1 (22C3) IHC stained slides of pre-treatment biopsied or resected materials were examined by previously reported image analysis techniques using e-Pathologist ® (NEC, Japan). Morphological characteristics of cancer cells (three and six parameters of nuclear shape and chromatin texture) were extracted as MC-scores. Of 11 cases (pilot cohort), PD-L1 IHC (22C3) and tumor mutation burden (TMB) by the NGS-based target sequence (NCC oncopanel ®) were examined. Correlation between MC-score, PD-L1 IHC, TMB status, and clinical outcome was calculated. A p-value of less than 0.05 was defined as statistically significant.
Decision tree analysis for evaluating predicting ICI-responsiveness was built using statistically significant MC-scores. We also tested the predictive value of a deep learning analysis (AI model) with 5-fold cross-validation. AUC (area under the curve) of ROC analysis was calculated.
Result
Of the responders, the MC-score of cancer cell were statistically different from those of the non-responders; nuclear texture contour complexity (11.8 vs. 8.25, median value of responder vs. non-responders; p<0.01), homogeneity (0.396 vs. 0.421; p<0.01), angular second moment (ASM) (0.0203 vs. 0.0214; p=0.049) and nuclear circularity (0.878 vs. 0.885, p=0.026). Circularity (p=0.011) and texture homogeneity (p=0.048) correlated with TMB. ASM texture correlated with PD-L1 expression (p=0.018). The decision tree model for predictive and screening purposes resulted in 0.83 and 0.62 accuracies, respectively. AUC of AI-model for ICI responsiveness resulted in fair (0.74 on average, range 0.55-0.81).
Conclusion
Our results indicate the substantial value of the morphological feature as a biomarker for ICI therapy. Morphological characteristics are eligible from archived FFPE samples, showed good correlation to the underlying genetic alteration. Digital pathology can serve useful predictive morphological biomarkers for precision medicine of lung cancer patients, and promising the power of AI-assisted pathology.
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
MS11 - Addressing Challenges with Surgical Resection of Lung Cancer (ID 74)
- Event: WCLC 2019
- Type: Mini Symposium
- Track: Treatment in the Real World - Support, Survivorship, Systems Research
- Presentations: 1
- Now Available
- Moderators:Ramon Rami-Porta, Haruhiko Kondo
- Coordinates: 9/09/2019, 15:45 - 17:30, Vancouver (2003)
-
+
MS11.03 - Minimizing Peri-Operative Morbidity with Pneumonectomy (Now Available) (ID 3502)
15:45 - 17:30 | Presenting Author(s): Shun-ichi Watanabe
- Abstract
- Presentation
Abstract
1. Introduction
The incidence of surgical morbidity after standard pneumonectomy is reportedly 30 to 60%. Many previous studies have addressed several risk factors for surgical morbidity after pneumonectomy, including age, cardiovascular disease, recent body weight loss, high smoking index, low FEV1.0 value, chronic obstructive pulmonary disease (COPD), right pneumonectomy, massive blood loss during surgery, long operation time, neoadjuvant therapy and so on. Although surgical morbidity after pneumonectomy easily lead to patients’ mortality. When pneumonectomy seems to be inevitable to remove the tumor, surgeons sometimes intraoperatively weigh the oncological benefit of pneumonectomy against the postoperative poor QOL and high morbidity rate.
In this paper, the cause and proper management of postpneumonectomy complications are discussed to minimize peri-operative morbidity with pneumonectomy as for especially following two life-threatening categories, cardiovascular and respiratory complications.
2. Type of Complications
2.1 Cardiovascular Complications
2.1.1 Supraventricular Arrhythmias
Most of supraventricular arrhythmias present 1 to 4 days after standard pneumonectomy, but it sometimes present even a week after surgery. The incidence of supraventricular arrhythmia after pneumonectomy is reportedly 4 to 25%. Risk factors for supraventricular arrhythmias include old age, right pneumonectomy, intrapericardial pneumonectomy, major co-morbidities, and so on. For patients who are considered to be high risk for postoperative atrial fibrillation, following prevention strategies are indicated. According to the 2014 AATS guidelines, continuing β blockers in patients taking β-blockers before surgery, using intravenous magnesium supplementation if serum magnesium levels are low, using diltiazem in those patients with preserved cardiac function who were not taking β-blockers preoperatively, or using amiodarone in patients at an intermediate to high risk of developing postoperative atrial fibrillation. For hemodynamically stable patients with new onset atrial fibrillation, intravenous β-blockers or calcium channel blockers are used to reduce a heart rate down to 100 beats per minute. When patients are hemodynamically unstable, direct current cardioversion should be used. And for patients with refractory atrial fibrillation, systemic anticoagulation therapy should be used carefully weighing benefits against the risk of bleeding, especially after EPP.
2.1.2 Ischemic Heart Disease
Ischemic heart disease is known to be an independent risk factor for severe complications after pneumonectomy. The risk of a myocardial infarction after pneumonectomy is reportedly approximately 0.2 to 2.1%. Patients who are candidates for pneumonectomy should undergo careful preoperative assessment to screen for untreated coronary ischemic disease.
2.1.3 Cardiac Herniation
Cardiac herniation is a rare complication after intrapericardial pneumonectomy. Patients develop cardiac herniation when the intrathoracic pressure changes rapidly by severe cough or vomit with decubitus position. Rapid and severe hemodynamic collapse following a change in patient positioning should heighten the clinical suspicion. Chest X-ray and electric cardiogram clearly show the abnormal position of the heart (Figure 1 and 2). Correction of the cardiac herniation should be conducted immediately by re-thoracotomy after successful resuscitation. Sewing the patch to the weak tissues around the pericardium rather than the pericardium itself after intrapericardial pneumonectomy could increase the risk of cardiac herniation.
2.2 Respiratory Complications
2.2.1 Pneumonia
The incidence of pneumonia after pneumonectomy is reportedly 2 to 10%. Since pneumonia after pneumonectomy could be a life-threatening complication, care must be taken to lessen the risk of pneumonectomy. Preoperative smoking cessation, chest physiotherapy by nurses or respiratory therapists, use of enough amount of post-thoracotomy painkillers, and bronchial toilet by bronchoscope are important practical factors for minimizing the risk of pneumonia.
2.2.2 Acute Respiratory Distress Syndrome (ARDS)
According to the previous literatures, ARDS occurs in 2.7 to 3.1% of patients after standard pneumonectomy with very high mortality of 50 to 70%. Treatment of ARDS is supportive. Mechanical ventilation with small tidal volumes of less than 6 mg/kg body weight should be used to minimize the barotrauma, and the FiO2 level should be decreased to the lowest level to minimize the oxidative trauma. There has been no evidence that steroids improve the prognosis of patients developing ARDS.
2.2.3 Bronchopleural Fistula (BPF)
The incidence of BPF, which is a life-threatening complication, is reportedly 2 to 11%. The mortality of BPF after pneumonectomy is very high rate of around 40%. Risk factors for BPF includes diabetes mellitus, malnutrition, long stump (especially for left side), right pneumonectomy, preoperative chemoradiation therapy, and so on. When a patient develop the BPF, open window technique should be applied to control thoracic cavity infection which can lead the patient to death.
3. Conclusion
The mortality and morbidity rates after pneumonectomy are very high compared with those after lobectomy, simply because the patients have less cardio-pulmonary reservations. Therefore, when complications occur, surgeons must aggressively treat them not to lose the patient with taking abovementioned knowledge into consideration.
Figure 1


Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
P1.09 - Pathology (ID 173)
- Event: WCLC 2019
- Type: Poster Viewing in the Exhibit Hall
- Track: Pathology
- Presentations: 1
- Moderators:
- Coordinates: 9/08/2019, 09:45 - 18:00, Exhibit Hall
-
+
P1.09-11 - Influences of Sampling Method to Morphological Feature Measurement of Lung Cancer Cell (ID 886)
09:45 - 18:00 | Author(s): Shun-ichi Watanabe
- Abstract
Background
Progress of imaging technologies in the field of histopathology enables us to exploit artificial intelligence (AI) techniques to detect cancer based on digital images for screening or quality assurance of diagnosis process. Nowadays, reports on the application of AI to cancer detection which claim 99-percent detection accuracy are found in every proceedings or journal of digital pathology. However, little attention has been paid to the influences of sampling method to AI-based histological diagnosis.
Method
Whole slide images of hematoxylin and eosin (H&E) stained slides collected from 94 non-small cell lung cancer (NSCLC) cases were captured by a virtual slide scanner (NanoZoomer, Hamamatsu Photonics, Japan). Sampling methods were needle biopsy (59 cases), operation (12 cases) and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) (29 cases). Regions of interest (ROI) were selected by an experienced pathologist. After selecting tumor cells only by AI-based tumor cell detecter (Figure.1), following morphological features were calculated: nuclear area, perimeter (Peri), circularity (Circ) and five texture features, i.e., angular secondary moment (ASM), contrast(Cont), homogeneity (Hom) and entropy (Ent) of gray level co-occurrence matrix (GLCM), and contour complexity (CC).
Result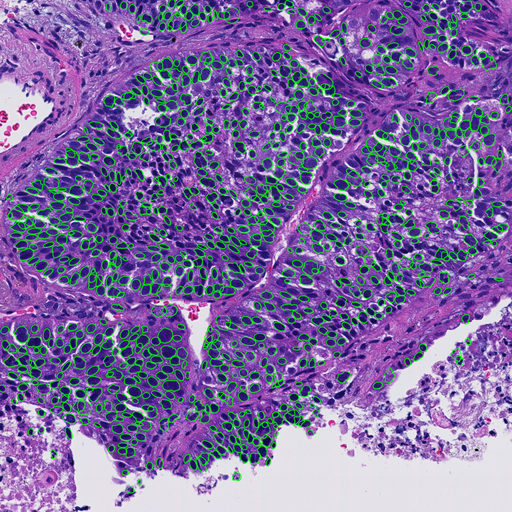
We found significant differences (p<0.05) in most of feature values except nuclear area and perimeter.
Conclusion
Our results suggest that methods of sampling significantly affect morphological feature values of nucleus and this fact must be taken into consideration when applying AI-based techniques to tissue image classification.
-
+
P1.11 - Screening and Early Detection (ID 177)
- Event: WCLC 2019
- Type: Poster Viewing in the Exhibit Hall
- Track: Screening and Early Detection
- Presentations: 1
- Moderators:
- Coordinates: 9/08/2019, 09:45 - 18:00, Exhibit Hall
-
+
P1.11-10 - Serum MicroRNA Biomarkers for Screening of Resectable Lung Cancer (ID 2253)
09:45 - 18:00 | Author(s): Shun-ichi Watanabe
- Abstract
Background
An accurate early screening method for lung cancer would be a powerful tool for decreasing lung cancer–related mortality. Computed tomography (CT) scanning is an effective method for lung cancer screening in high-risk populations. However, screening by CT scan has a limitation of low specificity (61%) for detection of lung cancer, resulting in unnecessary follow-up CT scans or invasive lung biopsies. In this study, we investigated the diagnostic potential of serum microRNAs (miRNAs) for detection of resectable lung cancer.
Method
Using the 3D-Gene® miRNA Labeling kit and the 3D-Gene® Human miRNA Oligo Chip (Toray Industries), we generated comprehensive miRNA profiles (expression levels of 2588 miRNAs) from 3744 serum samples obtained from 1566 patients with resectable lung cancer and 2178 participants with no cancer. We created a reliable diagnostic model for resectable lung cancer based on the combined expression levels of two miRNAs in the discovery set (208 lung cancer patients, 208 non-cancer participants). We then confirmed the diagnostic performance of the model in the validation set (1358 lung cancer patients, 1970 non-cancer participants).
Result
The combination of miR-A and miR-B yielded the best discrimination in the discovery set (AUC, 99.3; sensitivity, 99.0%; specificity, 99.0%). We then confirmed the diagnostic performance of the model in the validation set, and showed that the model was accurate (AUC, 0.973; sensitivity, 95.0%; specificity, 99.0%). According to univariable logistic regression analysis, the odds ratio of the diagnostic model for the presence of lung cancer was 21.76 (95% confidence interval [CI], 15.98–29.63). The diagnostic index exhibited high performance for all pathological stages (IA, 96.1%; IB, 93.7%; IIA, 97.3%; IIB, 96.7%; IIIA, 90.2%; IIIB, 83.3%; IV, 100%), and histological types (adenocarcinoma, 95.1%; squamous cell carcinoma, 94.2%; small-cell lung cancer, 90.9%).
Conclusion
A comprehensive analysis of serum levels of 2588 miRNAs in 1566 patients with lung cancer and 2178 non-cancer participants identified a combination of two miRNAs that could reliably detect resectable lung cancer. This study was the largest of its kind performed to date, and the results confirm that evaluation of serum miRNAs is an effective method for detection of resectable lung cancer. The high sensitivity and specificity of this screening model could help to decrease lung cancer–related mortality, as well as the number of unnecessary follow-up CT scans and invasive lung biopsies.
-
+
P1.17 - Treatment of Early Stage/Localized Disease (ID 188)
- Event: WCLC 2019
- Type: Poster Viewing in the Exhibit Hall
- Track: Treatment of Early Stage/Localized Disease
- Presentations: 1
- Moderators:
- Coordinates: 9/08/2019, 09:45 - 18:00, Exhibit Hall
-
+
P1.17-37 - Minimally Invasive Open Surgery (MIOS) for Clinical Stage I Lung Cancer: Perioperative Outcomes in Recent 5 Years (ID 1638)
09:45 - 18:00 | Author(s): Shun-ichi Watanabe
- Abstract
Background
Many thoracic surgeons have tried to make lung cancer surgery less invasive. Although several minimally invasive procedures for lung cancer surgery have been proposed, it has been controversial which procedure is the most optimal. Since around 2010, minimally invasive open surgery (MIOS) has been adopted for lung cancer surgery at our institute. MIOS was performed with direct vision and thoracoscopic vision through a 2-cm port and a muscle-sparing mini-thoracotomy (incision, 6-8 cm in the fourth or fifth intercostal space at the anterior or posterior axillary line). The objective of this study was to evaluate MIOS in terms of perioperative outcomes in recent 5 years.
Method
Between 2013 and 2017, 2404 patients underwent pulmonary resection for lung cancer at National Cancer Center Hospital, Tokyo, Japan. Among them, 1930 patients with clinical stage I lung cancer were included in this study. We investigated several perioperative factors according to the type of pulmonary resection: lobectomy, segmentectomy and wedge resection.
Result
The patients consisted of 993 men (51.5%) and 937 women (48.5%) with a median age of 69 years (range: 32-90 years). Lobectomy was performed in 1288 patients (66.7%), segmentectomy in 397 (20.6%), and wide wedge resection in 245 (12.7%). Median blood loss was 32 ml (range: 1-1489 ml) for lobectomy, 20 ml (range: 1-435 ml) for segmentectomy, and 4 ml (range: 1-177 ml) for wedge resection. Median operative time was 122 min (range: 45-293 min) for lobectomy, 115 min (range: 69-211 min) for segmentectomy, and 66 min (range: 29-177 min) for wedge resection. Median length of post-operative hospital stay was 4 days (range: 1-57 days) for lobectomy, 4 days (range: 2-20 days) for segmentectomy, and 3 days (range: 2-24 days) for wedge resection. There were no operative deaths. The morbidity rate was 11.8% for lobectomy, 7.3% for segmentectomy, and 4.1% for wedge resection. The 30-day mortality rate was 0.16% for lobectomy, 0.25% for segmentectomy, and 0% for wedge resection.
Conclusion
MIOS for clinical stage I lung cancer is a technically safe and feasible procedure with a low complication rate and a shorter hospital stay. The oncological outcomes with a longer follow-up need to be investigated.


