Virtual Library
Start Your Search
Georgios Tsakonas
Author of
-
+
P2.13 - Targeted Therapy (Not CME Accredited Session) (ID 962)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.13-02 - ALK-Translocation and Brain Metastases: A Retrospective Study. Correlation Between Clinical Outcome, Disease Burden and Management. (ID 12949)
16:45 - 18:00 | Author(s): Georgios Tsakonas
- Abstract
Background
Brain metastases from non‐small cell lung cancer is often regarded as the ominous sign of disease progression .
In the ALK-translocated population, brain metastases are seen in a higher incidence, either at diagnosis or as a common site of progression for patients receiving tyrosine kinase inhibitors (TKI).
The management of brain metastases in this population remains a challenge since several methods of treatment are available. TKI-treatment, especially with second or third generation drugs can be effective but the role of radiation therapy, with either whole brain radiotherapy (wbrt) or stereotactic radiosurgery (srs), has not been fully elucidated.
A retrospective study was conducted at ou Institution in order to evaluate the frequency of brain metastases in this subggroup of patients and in order to explore clinical features associated with survival.
a9ded1e5ce5d75814730bb4caaf49419 Method
88 consecutive patients with advanced ALK+ adenocarcinoma were treated at our institution. during the perod 2011-2018. Data on CNS imaging modality, treatment strategy and outcome was collected by chart review.
4c3880bb027f159e801041b1021e88e8 Result
Cns-imaging with either MRI or CT (in 38% and 62% of the cases respectively) was performed in 73 cases. 44 patients (61%) were found to have CNS metastases (Male/female ratio 48/52%; median age 60y).
23% were found at the time of primary cancer diagnosis, 36% on time of PD on chemotherapy, 34% on PD on crizotinib and 7% at PD on 2nd gen ALKinh .
27% of the patients had 1-3 metastases, 34% 4-10 met and 39 % >10.
Pharmacological treatments in the group as a whole: chemotherapy (n=38); crizotinib (n=35); alectinib (n=10); ceritinib (n=20); brigatinib (n=3), lorlatinib (n=1).
Radiotherapy was administered in 57% as either SRS or WBRT (52/48%) .
Treatment strategies upon discover of CNS-metastes: Radiotherapy solely 27%, combination of radiotherapy and pharmacological treatment in 25%, switch to crizotinib and to 2nd gen ALKi in 18 and13 % respectively.
Median OS from the diagnosis of CNS metastasis was 29months (95% CI 11-59). 1- and 2-year survival was 61% and 51%, respectively.
Neither gender, age, timing for diagnosis of CNS metastases nor the use of radiotherapy were significant prognostic factors for OS (Cox proportional hazard analysis).
Use of 2nd gen ALKin as treatment strategy seemed to be superior to crizotinib and radiotherapy alone even if median OS not yet was reached.
8eea62084ca7e541d918e823422bd82e Conclusion
The high incidence of CNS metastases in this subpopulation of patients (Caucasian with advanced ALK+ NSCLC) was confirmed in this study. The wider implementation of 2nd generation ALKi in clinical practice will probably change the prognosis of these subjects.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.12 - Small Cell Lung Cancer/NET (Not CME Accredited Session) (ID 978)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.12-17 - A Retrospective Study Examining the Role of PET-CT in the 8<sup>th</sup> TNM Staging System of SCLC (ID 12873)
12:00 - 13:30 | Author(s): Georgios Tsakonas
- Abstract
Background
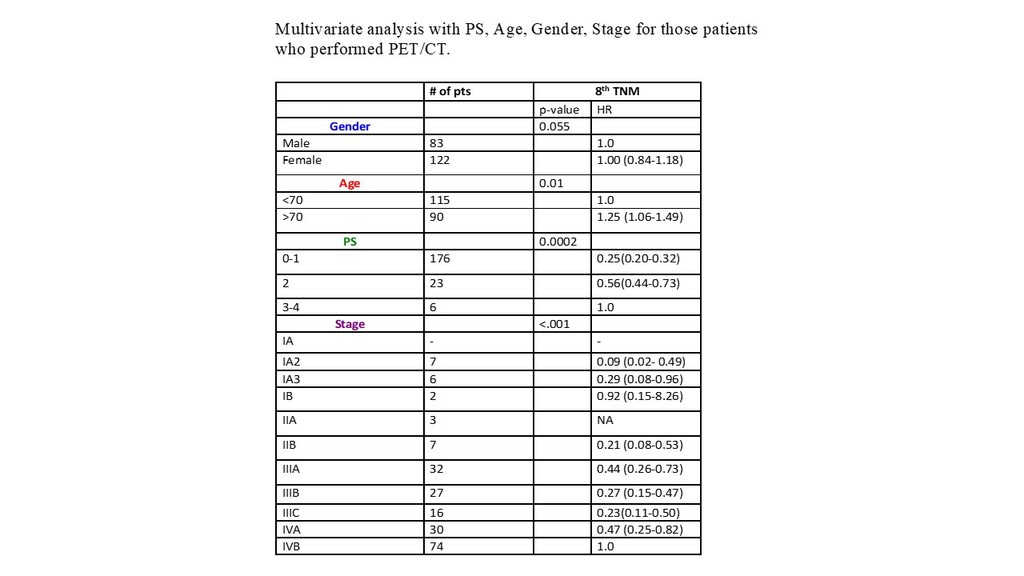
We have recently performed a validation of the 8th TNM system in SCLC. The aim of the present study is to perform a subgroup analysis on patients (pts) who underwent a PET/CT scan, to furhter assess potential utility of this method in SCLC pts, since PET/CT is usually performed primarily to identify potentially curable cases.
a9ded1e5ce5d75814730bb4caaf49419 Method
Between January 2008 and February 2016, a total of 706 pts with SCLC were diagnosed in the Stockholm and Gotland region. A multivariate model adjusted for basic patient characteristics and PET-CT was performed.
4c3880bb027f159e801041b1021e88e8 Result
One third of the patients had performed a PET/CT scan (n=204). Pts were classified according to the 8th TNM. The table shows patient distrubution according to clinical variables and stage (8th TNM), as well as HR for multivariate survival analysis. Many pts (48%) were classified to stage I-III disease, while the rest had stage IV. Pts with stage I-III were treated with Surgery (n=13), Radiotherapy+ Chemotherapy (CT) (n=80) or Stereotactic body radiation (n=7). The patients who were diagnosed with stage IV disease were treated with palliative CT or did not receive any oncological therapy. In pts that did not perform PET/CT, the majority (87%) were treated with CT or did not receive treatment. The percentage of pts diagnosed with M1b-disease was slighlty higher in those who performed a PET/CT vs those who did not (7% vs 3%, respectivley).
8eea62084ca7e541d918e823422bd82e Conclusion
The 8th TNM edition has a strong prognostic impact in SCLC. Incorporating a PET/CT scan in the diagnostic workup of SCLC is relevant to distinguish potentially curable pts (stages I-III) from pts with stage IV disease, and may be of value to indentify single extra-thoracic metastases (M1b cases).
6f8b794f3246b0c1e1780bb4d4d5dc53


