Virtual Library
Start Your Search
Osamu Kawamata
Author of
-
+
P2.09 - Pathology (Not CME Accredited Session) (ID 958)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.09-30 - Clinicopathological Investigation of Four Resected Cases for Pleomorphic Carcinoma of the Lung (ID 12835)
16:45 - 18:00 | Author(s): Osamu Kawamata
- Abstract
Background
Pleomorphic carcinoma (PC) of the lung has a poor prognosis and no established standard treatment. Particularly, cases of recurrence after surgery often result in death within one year of recurrence. At our hospital, we experienced four cases of PC, and all these patients remain alive, including those with recurrence. We report these cases of PC together with our histopathological findings.
a9ded1e5ce5d75814730bb4caaf49419 Method
We examined four patients with PC who underwent thoracoscopic lobectomy and mediastinal lymph node dissection between October 2014 and March 2017. The histopathological findings were expression of programmed death ligand 1 (PD-L1) and CD8-positive tumor-infiltrating lymphocytes (CD8+TILs), which were examined for their relationship with prognosis. The expression of CD8+TILs was evaluated using the ratio of CD8+/CD45+ (leukocyte common antigen) TILs.
4c3880bb027f159e801041b1021e88e8 Result
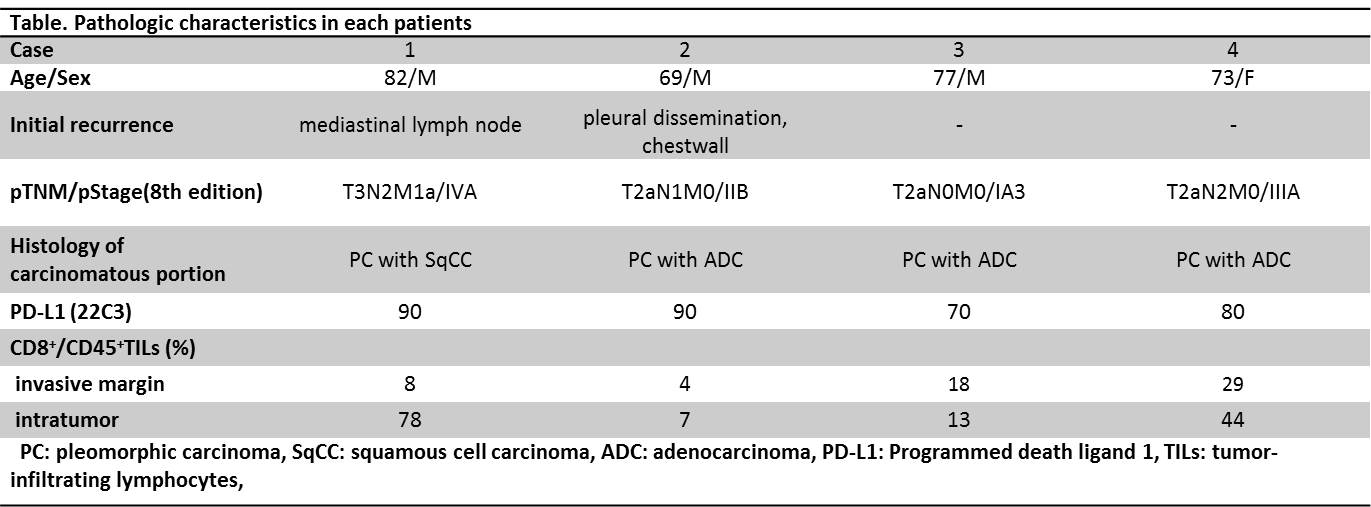 While all patients survived, two of four patients experienced recurrence. Case 1 experienced recurrence 5 months after surgery and remains currently alive 35 months after recurrence using radiation therapy alone. Case 2 developed pleural dissemination and recurrence 10 months after surgery and remains alive 29 months after recurrence with a good partial response to chemotherapy and immune checkpoint inhibitors (nivolumab). Case 3 and 4 are both alive without recurrence 28 months and 12 months after surgery, respectively. All cases have high PD-L1 expression (tumor proportion score >50%) and the CD8+/CD45+TILs ratio demonstrated a trend toward a higher expression in intratumor than invasive margin. Case 2 showed a good response to immune checkpoint inhibitors, despite the expression of CD8+TILs was the lowest of four patients. Case 4 had high expression of CD8+TILs, which might be associated with good prognosis in spite of locally advanced cancer.
While all patients survived, two of four patients experienced recurrence. Case 1 experienced recurrence 5 months after surgery and remains currently alive 35 months after recurrence using radiation therapy alone. Case 2 developed pleural dissemination and recurrence 10 months after surgery and remains alive 29 months after recurrence with a good partial response to chemotherapy and immune checkpoint inhibitors (nivolumab). Case 3 and 4 are both alive without recurrence 28 months and 12 months after surgery, respectively. All cases have high PD-L1 expression (tumor proportion score >50%) and the CD8+/CD45+TILs ratio demonstrated a trend toward a higher expression in intratumor than invasive margin. Case 2 showed a good response to immune checkpoint inhibitors, despite the expression of CD8+TILs was the lowest of four patients. Case 4 had high expression of CD8+TILs, which might be associated with good prognosis in spite of locally advanced cancer.
8eea62084ca7e541d918e823422bd82e Conclusion
The expression of CD8+TILs may be associated with prognosis of PC. We plan to continue investigating how PD-L1 expression and the CD8+TILs ratio are related to recurrence and therapeutic response.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P2.15 - Treatment in the Real World - Support, Survivorship, Systems Research (Not CME Accredited Session) (ID 964)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.15-11 - Clinical Outcome of Pulmonary Resection for Non–Small Cell Lung Cancer in Extremely Elderly Patients (85-Year-Old or Over) (ID 14137)
16:45 - 18:00 | Author(s): Osamu Kawamata
- Abstract
Background
Surgical resection is considered to be an effective therapy in the elderly patients. In Japan, the number of surgical operations performed in the elderly patients has been increasing. We reviewed the outcome of surgical treatment and the determining indication of pulmonary surgery in patients aged 85 years or over.
a9ded1e5ce5d75814730bb4caaf49419 Method
We performed surgical resection for 27 lung cancer patients aged 85 years or over in our hospital from January 2007 to December 2016. The patients’ operative procedure, histological type, comorbidity, surgery-related complications, prognosis, and recurrence were retrospectively reviewed. We performed pulmonary surgery for elderly patients who have to be able to undergo pulmonary physiotherapy, have good performance status (0-1 in ECOG scale), and be free from psychological disorder such as dementia.
4c3880bb027f159e801041b1021e88e8 Result
There were 19 males and 8 females. Their mean age was 87.0 years (range: 85-93 years). The mean follow-up period after operation was 1585 days (range: 395-3255 days). Operative procedures include lobectomy (N=10), segmentectomy (N=8), and wedge resection (N=9). Histological type include adenocarcinoma (N=18), squamous cell carcinoma (N=7), adenosquamous carcinoma (N=1), and LCNEC (N=1). Pathological stage was ⅠA in 20 patients, ⅠB in 4patients, ⅡB in 2 patients, and ⅢA in 1 patient. 17 patients had comorbidity including coincidence of other malignancy, anti-coagulant therapy, history of the lobectomy, and others. No patients died from surgery or post-surgical complications. Morbidity rate was 14.8% (e.g. refractory pulmonary fistula, Atrial fibrillation, heart failure, atelectasis). 14 patients are alive, whereas 11 patients died from other diseases than lung cancer. 4 patients experienced recurrence, and 2 patients of those died. 5-year survival rate was 71.4%, and 3-year survival rate was 87.5%.
8eea62084ca7e541d918e823422bd82e Conclusion
Our study indicates that the surgical resection of non-small cell lung cancer benefits patients, even with extremely elder age (85-year-old or older). We consider patients with clinical stageⅠ are good candidates. The long-term prognosis is expected if we chose the patients in elderly people lung cancer definitely.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.16 - Treatment of Early Stage/Localized Disease (Not CME Accredited Session) (ID 982)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.16-28 - Surgery of Stage I Non-Small Cell Lung Cancer in Patients Aged 70 Years or Older (ID 12259)
12:00 - 13:30 | Presenting Author(s): Osamu Kawamata
- Abstract
Background
Non-small cell lung cancer (NSCLC) is a typical disease of the elderly patients, and is becoming increasingly. Surgical resection is standard treatment for early-stage NSCLC. The strong predictor of long-term survival for lung cancer is reported to be age. We evaluate the influence of age for stage I non- small cell lung cancer in elderly patients 70 years or older.
a9ded1e5ce5d75814730bb4caaf49419 Method
156 cases with stage I (UICC 8th) non-small cell lung cancer aged 70 years or more who underwent surgery at our hospital between 2007 and 2016 were studied. The patients’ medical records were reviewed with age, gender, type of operation, postoperative morbidity, postoperative mortality and survival results.
4c3880bb027f159e801041b1021e88e8 Result
There were 89 male and 67 female. The average ages were 78.2years (range, 70-90 years). The 5-year survival of all patients was 75.7%. Two groups were compared: patients aged 70 to 79 years, patients aged 80 years or more. At pathologic analysis, 74.5% and 70.7% were stage IA, 25.5% and 29.3% were stage IB. Procedure performed was lobectomy in 52.1% and 39.7%, segmentectomy in 40.8% and 39.7%, and wedge resection in 7.1% and 20.7%. Postoperative complications were documented in 12 patients (12.2%) and 11patients (19.0%) without any difference in two groups. The 30-day mortality was 0.6% , and the 90-day mortality was 0.6% . No case died for lung cancer and 14 cases (male 11) died for other disease within 5 years after lung resection in 70-79 years. The 5-year survival was 81.3%. 3 cases died for lung cancer and 12 cases (male 8) died for other disease within 5 years after lung resection in 80 years or more. The 5-year survival was 66.3%. Comparing the 5-year survival by male and female at 5 year interval were 90.0% and 90.2% in 70-74 years, 68.5% and 90.5% in 75-79 years, 61.1% and 88.9% in 80-84 years, and 82.5% and 25.0% in 85 years or more. The reason for the poor prognosis of patients in 75-79 years, 80-84 years male and 85 years or more female was that many deaths by other disease occur.
8eea62084ca7e541d918e823422bd82e Conclusion
Lung resection for stage I NSCLC patients in 70 years or more expected long-term survival. However, the cause of death was found to be more death from other disease than lung cancer after lung resection. We thought that the management of other disease improved the prognosis after lung resection for stage I NSCLC in elderly patients aged 70 years or older.
6f8b794f3246b0c1e1780bb4d4d5dc53


