Virtual Library
Start Your Search
Chee-Shee Chai
Author of
-
+
P1.15 - Treatment in the Real World - Support, Survivorship, Systems Research (Not CME Accredited Session) (ID 947)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.15-15 - Real-World Experience with Afatinib after Failure of First-Generation Epidermal Growth Factor Receptor-Tyrosine Kinase Inhibitor (ID 13652)
16:45 - 18:00 | Author(s): Chee-Shee Chai
- Abstract
Background
Afatinib, a second-generation epidermal growth factor receptor (EGFR)-tyrosine kinase inhibitor (TKI) is the recommended first-line treatment for patients with advanced non-small cell lung cancer harbouring sensitizing EGFR mutations. The role of afatinib after failure of first-generation EGFR-TKIs is controversial.
a9ded1e5ce5d75814730bb4caaf49419 Method
A retrospective observational study of patients with EGFR mutant advanced NSCLC receiving second-line afatinib after failure of first-generation EGFR-TKI in University Malaya Medical Center from 1st December 2014 to 30th April 2018.
4c3880bb027f159e801041b1021e88e8 Result
The demographic and clinical characteristics of 27 patients treated with afatinib after failure of first-generation EGFR-TKI are shown in Table 1. Twenty-three patients received gefitinib and 4 patients received erlotinib as first-line treatment. The mPFS with first-line treatment was 11.9 months. Fifteen patients had progression of disease (PD) following second-line afatinib with mPFS of 4.2 months and median time-to-treatment failure of 5.7 months. The mPFS2 conferred by first-line first-generation EGFR-TKI and second-line afatinib was 18.4 months. The overall response rate to second-line afatinib was 18.5% (5/27) while the disease control rate as 70.3% (19/27).
Two patients who had PD on first-generation EGFR-TKI due to T790M mutation received second-line afatinib while waiting for compassionate access to osimertinib. Nine of the 15 patients (69.2%) with PD on afatinib underwent investigations for resistance mechanisms. Three patients had T790M mutation, one of whom had concomitant small cell lung cancer transformation. c-MET amplification was detected in another 3 patients. One patient each had EML4-ALK rearrangement and epithelial mesenchymal transition.
8eea62084ca7e541d918e823422bd82e Conclusion
Afatinib conferred a modest mPFS benefit after failure of first-generation EGFR-TKI. The mPFS of sequential treatment with first-generation EGFR-TKI followed by afatinib seems longer than the mPFS of first-line afatinib in phase 3 randomised controlled trials. Apart from T790M mutation, the resistance mechanisms to second-line afatinib in our patients are more heterogenous.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.13 - Targeted Therapy (Not CME Accredited Session) (ID 979)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.13-15 - First-Line Afatinib Dose Initiation and Adjustment in Patients with EGFR Mutant Advanced Non-Small Cell Lung Cancer (ID 13746)
12:00 - 13:30 | Author(s): Chee-Shee Chai
- Abstract
Background
The recommended starting dose of afatinib is 40mg od with 20mg, 30mg and 50mg tablets available for dose adjustment.
a9ded1e5ce5d75814730bb4caaf49419 Method
This is a retrospective observational study of starting dose, dose adjustment and optimal dose of first-line afatinib in patients with EGFR mutant advanced non-small cell lung cancer in University Malaya Medical Center from 1st December 2014 to 30th April 2018.
4c3880bb027f159e801041b1021e88e8 Result
Of 22 patients on first-line afatinib, the starting dose was 40 mg od in 12 patients and 30 mg od in 10 patients (Figure 1). Among the 12 patients started on afatinib 40mg od, 4 (33.3%) did not require dose adjustment, 4 (33.3%) needed dose reduction to 30mg od, 2 (16.7%) needed dose reduction to 20mg od, and 2 (16.7%) had dose escalation to 50mg od. Among 10 patients started on afatinib 30mg od, 6 (60%) did not require dose adjustment, 1 (10%) needed dose reduction to 25mg od and 3 (30%) had dose escalation to 40mg od.
Dose reduction was to reduce the cost of treatment in 1 patient and to reduce drug-related side-effects in the rest. Dose escalation was exclusively to improve disease control. The overall response rate and disease control rate was 80% (8/10) and 90% (9/10) in patients who did not require dose adjustment; while the respective rates were 85.7% (6/7) and 100% (7/7) in patients who had dose reduction.
The optimal dose of afatinib defined by good disease control and tolerable side-effects was 50mg od in 9.1% (2/22), 40mg od in 31.8% (7/22), 30mg od in 31.8% (7/22), 25mg od in 13.6% (3/22) and 20mg od in 13.6% (3/22) of patients.
8eea62084ca7e541d918e823422bd82e Conclusion
We suggest starting afatinib at 30mg od and adjust the dose accordingly because dose adjustment is not required in most cases on this starting dose and it is the commonest optimal dose.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.15 - Treatment in the Real World - Support, Survivorship, Systems Research (Not CME Accredited Session) (ID 981)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.15-21 - Real-World Experience of First-Line Afatinib Treatment in Patients with EGFR Mutant Advanced Non-Small Cell Lung Cancer (ID 13600)
12:00 - 13:30 | Author(s): Chee-Shee Chai
- Abstract
Background
Published reports of first-line afatinib treatment efficacy, side-effects and resistance mechanism in the real-world setting are lacking.
a9ded1e5ce5d75814730bb4caaf49419 Method
A retrospective observational study of patients with EGFR mutant advanced non-small cell lung cancer (NSCLC) receiving first-line afatinib in University Malaya Medical Center from 1st December 2014 to 30th April 2018.
4c3880bb027f159e801041b1021e88e8 Result
Twenty-two of 33 patients on first-line afatinib were eligible for analysis. The patients’ demographic and clinical characteristics are as shown in Table 1. The mPFS was 14.3 months, overall response rate was 86.3% (19/22) and disease control rate was 95.5% (21/22). The median time-to-treatment failure was 16.2 months. The median overall survival has not been reached but 12-month survival rate was 81.8% (18/22).
A patient with exon 18 G719X and exon 20 S768I mutation had received treatment for 23.3 months without disease progression (PD). The PFS of a patient with exon 20 insertion was 9 months and of another patient with exon 18 G719X and exon 20 T790M mutations was 4.4 months. Of patients with brain metastases, the PFS of 2 patients treated with stereotactic radiosurgery (SRS) was 15.9 months and 9 months, respectively while that of a patient who had whole brain radiotherapy (WBRT) and a patient who underwent debulking surgery only was 16.5 months and 2.6 months, respectively.
The incidence of side-effects was rash 90.1% (20/22), stomatitis 63.3% (14/22), paronychia 72.7% (16/22), and diarrhea 77.3% (17/22). One (4.5%) patient each had grade 3 diarrhea and cutaneous lesions. Of 17 patients with PD, 2 (11.8%) had PD in the brain. T790M mutation was detected in 62.2% (8/13) patients who underwent repeat biopsy.
8eea62084ca7e541d918e823422bd82e Conclusion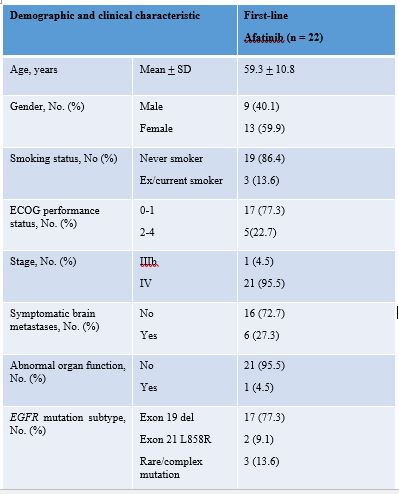
Afatinib is an effective treatment of EGFR-mutant advanced NSCLC. When combined with SRS or WBRT, afatinib conferred good PFS in patients with symptomatic brain metastases. Severe side effects are uncommon and T790M mutation was the commonest resistance mechanism.
6f8b794f3246b0c1e1780bb4d4d5dc53


