Virtual Library
Start Your Search
Yutthaphan Wannasopha
Author of
-
+
P1.14 - Thymoma/Other Thoracic Malignancies (Not CME Accredited Session) (ID 946)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.14-27 - Differentiation Between Each Thymic Epithelial Tumor According to WHO Classification Scheme by Using MDCT Findings (ID 12216)
16:45 - 18:00 | Presenting Author(s): Yutthaphan Wannasopha
- Abstract
Background
Thymic epithelial tumors are the uncommon mediastinal tumors but are the most common primary tumors of the anterior mediastinum. Computed tomography (CT) is the imaging modality of choice for assessment in patients suspected thymic epithelial tumor. The objectives of this study were to assess the CT features of various types of thymic epithelial tumors on the basis of the 2004 WHO classification and to identify the specific CT findings for differentiation between each thymic epithelial tumor.
a9ded1e5ce5d75814730bb4caaf49419 Method
A retrospective study reviewed CT findings of 35 patients with thymic epithelial tumors, who underwent surgical resection from January 2010 to April 2017 and had available pre-operative chest CT study. The tumors were reclassified into six types of thymic epithelial tumors (A, AB, B1, B2, B3 and thymic carcinoma) on the basis of the 2004 WHO classification system. The CT findings including the size (longest diameter), margin, shape, presence of focal area of low attenuation of necrosis or cystic change, mediastinal fat invasion, great vessels invasion, degree and pattern of tumor enhancement, presence of tumor calcification and presence of mediastinal lymphadenopathy (short axis diameter more than 10 mm), the presences of pleural effusion, pleural mass, pulmonary nodule, pericardial effusion and extrathoracic metastasis were evaluated.
4c3880bb027f159e801041b1021e88e8 Result
Our study consisted of 20 (57.14%) men and 15 (42.86%) women, age 15-78 years (mean 51.25 years). Pathological proven into 30 thymomas (85.71%) and 5 cases (14.29%) of thymic carcinomas. The 30 thymomas were classified according to WHO classification; type A in 5 (14.29%), type AB in 4 (11.43%), type B1 in 5 (14.29%), type B2 in 9 (25.71%), and type B3 in 7 (20%) patients. The tumor sizes of type A, AB, B1, B2 & B3 thymomas and thymic carcinoma were 6.2±1.97, 8.1±2.17, 4.9±2.47, 6.8±3.04, 4.7±1.87, and 9.6±2.78 cm, respectively. No definite CT manifestation that distinguishes between each different WHO pathological type of thymoma with statistical significance. The tumor dimension > 8 cm, irregular margin, mediastinal fat invasion, great vessel invasion, lymphadenopathy, pericardial effusion and extrathoracic metastasis could differentiate between thymoma and thymic carcinoma (P-value <0.05). Great vessel invasion and extrathoracic metastasis had high sensitivity (80%), specificity (100%), PPV (100%) and NPV (96.77%) for diagnosis thymic carcinoma.
8eea62084ca7e541d918e823422bd82e Conclusion
No definite CT manifestation that distinguishes between each different WHO pathological types of thymomas. Tumor size more than 8 cm, irregular margin, presence of mediastinal fat invasion, great vessel invasion, mediastinal lymphadenopathy or extrathoracic metastasis favors the diagnosis of thymic carcinoma.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P1.16 - Treatment of Early Stage/Localized Disease (Not CME Accredited Session) (ID 948)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.16-57 - Outcomes of Pulmonary Resection in Elderly Non-Small Cell Lung Cancer Patient (ID 11989)
16:45 - 18:00 | Author(s): Yutthaphan Wannasopha
- Abstract
Background
Because of increasing in life span and more than third-fourth of lung cancer patients being age > 60-65 years old, appropriate treatment of old lung cancer patients has become an important issue. The aim of this study is to evaluate the short and long-term surgical outcomes in elderly patients, and to identify prognostic factors of overall mortality.
a9ded1e5ce5d75814730bb4caaf49419 Method
Medical records of patients with non-small cell lung cancer (NSCLC) who underwent pulmonary resection at Chiang Mai University Hospital from January 2002 through December 2016 were retrospectively reviewed. Patients were divided into two groups; age less than 70 years (non-elderly group) and 70 years or more (elderly group). Primary outcome was major post-operative complications and in-hospital death; secondary outcome was long-term survival. Logistic regression and cox proportional hazard model were used to analyze data.
4c3880bb027f159e801041b1021e88e8 Result
This study included 583 patients; 167 in elderly group, and 416 in non-elderly group. Patients in elderly group were more likely to have government insurance, be active smoker, and have a diagnosis of COPD, an abnormal ECG, to undergo a sublobar resection, lymph node sampling, and no chemotherapy treatment than those in the non-elderly group. There were no differences in term of in-hospital mortality, composite post-operative complications, and overall mortality. At multivariable analysis, the composite post-operative complications in the elderly group was not statistically different from the non-elderly group (Adjusted odd ratios = 0.52, 95% CI=0.21-1.28), however the elderly group was more likely to die (HRadj)=2.44, 95%CI=1.26-4.74). Adverse prognostic factors for overall mortality in elderly patients were a poorly differentiated tumor (HRadj=3.53, 95%CI=1.45-8.61) and the presence with perineural invasion (HRadj=3.95, 95%CI=1.14-13.77)
Table 1 prognostic factors for overall mortality of elderly NSCLC patients after pulmonary resection
Variables
Hazard Ratio
95% CI
p-value
Male vs Female
1.43
0.62-3.26
0.401
Smoking amount
≥20 pack-year
0.91
0.45-1.82
0.783
Stage of cancer
Stage I
1.00
Reference
Stage II
0.76
0.36-1.57
0.452
Stage III
2.18
0.92-5.16
0.077
Stage IV
1.70
0.53-5.46
0.373
Grading of cell differentiation
Well
1.00
Reference
Moderately
0.80
0.39-1.67
0.558
Poorly
3.53
1.45-8.61
0.006
Undifferentiated
1.72
0.41-7.31
0.462
Intratumoral lymphatic invasion
2.73
0.99-7.52
0.052
Intratumoral vascular invasion
1.76
0.91-3.39
0.092
Perineural invasion
3.95
1.14-13.77
0.031
SLND versus SLNS
0.51
0.24-1.10
0.084
Chemotherapy
No chemotherapy
1.00
Reference
Adjuvant or induction therapy
0.69
0.33-1.46
0.330
1st-line treatment
0.76
0.15-3.80
0.734
Sublobar resection versus lobectomy
1.78
0.65-4.90
0.261
8eea62084ca7e541d918e823422bd82e Conclusion
Surgery in elderly NSCLC is a safe procedure. Patients presenting with perineural invasion and poorly differentiated tumor should be further considered for possible adjuvant treatment.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P2.15 - Treatment in the Real World - Support, Survivorship, Systems Research (Not CME Accredited Session) (ID 964)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.15-28 - Effect of Insurance Types on Tumor Recurrence and Overall Survival in Resectable Non-Small Lung Cancer Patients in Northern Thailand (ID 12375)
16:45 - 18:00 | Author(s): Yutthaphan Wannasopha
- Abstract
Background
The effect of insurance types on tumor recurrence and overall survival in resectable non-small cell lung cancer in northern Thailand have never been reported. The aim of this study is to identify the association between Thailand’s insurance types and long-term outcomes of treatment.
a9ded1e5ce5d75814730bb4caaf49419 Method
Medical records of patients with non-small cell lung cancer (NSCLC) who underwent pulmonary resection at Chiang Mai University Hospital from January 2002 through December 2016 were retrospectively reviewed. Patients were divided into two groups; patients with National Health Security insurance (NHSI) and patients with Government/State Enterprise insurance or private insurance (GEI). Patient characteristics, pathologic findings and long-term outcomes were assessed. Primary outcome was overall survival; secondary outcome was tumor recurrence. Multivariable cox’s regression analysis were used to analyze data.
4c3880bb027f159e801041b1021e88e8 Result
This study included 583 patients; 344 with NHSI and 239 with GEI. Patients with NHSI were more likely to be active smokers, lower % predicted FEV1, present with higher stage tumor, having moderately and poorly differentiated tumor, present with tumor necrosis, and undergo open surgical approach than those with GEI. There were no differences between the two groups in term of lymph node dissection, chemotherapy and post-operative complications. At multivariable analysis, tumor recurrence in patients with GEI was not statistically different from what observed in patients with NHSI (adjusted hazard ratio (HRadj)=1.03, 95% CI=0.51-2.11), however patients with NHSI was more likely to die (HRadj=2.45, 95%CI=1.11-5.42).
8eea62084ca7e541d918e823422bd82e Conclusion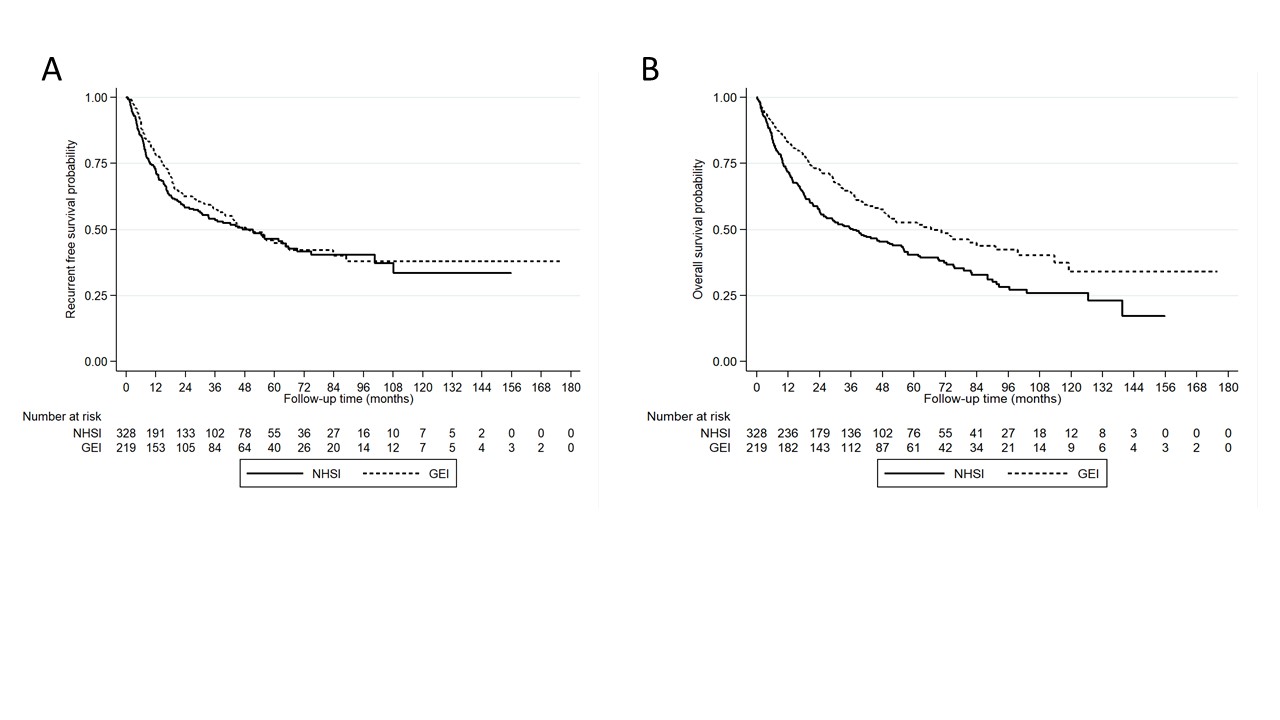
Thai NSCLC patients with NHSI coverage were more likely to experience shorter overall survival than those with GEI. The difference in medical coverage in each type of insurance, especially in term of regimens of chemotherapy, targeted therapy and immunotherapy may be associated with overall survival of patients. The Thai government should take into account this difference.
6f8b794f3246b0c1e1780bb4d4d5dc53


