Virtual Library
Start Your Search
Jia Wang
Author of
-
+
P1.05 - Interventional Diagnostics/Pulmonology (Not CME Accredited Session) (ID 937)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.05-23 - Evaluation of the 8th Edition of the TNM Classification for Lung Cancer at a Single Institution (ID 13730)
16:45 - 18:00 | Presenting Author(s): Jia Wang
- Abstract
Background
The 7th edition has been used more than10 y ears and has proven reliable, but various problems had been indicated.The latest (8th) edition of the lung cancer staging classification was published in 2017. The purpose of this retrospective study is to make a external validation to the 8th edition of the lung cancer staging system.
a9ded1e5ce5d75814730bb4caaf49419 Method
Subjects included 3,229 patients who underwent pulmonary resection for primary non-small cell lung cancer.Survival characteristics were compared using the 7th and 8th editions of the staging system.
4c3880bb027f159e801041b1021e88e8 Result
8eea62084ca7e541d918e823422bd82e Conclusion
 According to the 7th edition, there was no significant difference between pStages IIB and IIIA(P = 0.650), however, according to the 8th edition, there were significant differences between each adjacent stage group. Moreover, to the T descriptor(tumor size), which got most emphasis in the 8th edition, there were significant differences between each adjacent pT classification, either according to the 7th edition or the 8th edition.
According to the 7th edition, there was no significant difference between pStages IIB and IIIA(P = 0.650), however, according to the 8th edition, there were significant differences between each adjacent stage group. Moreover, to the T descriptor(tumor size), which got most emphasis in the 8th edition, there were significant differences between each adjacent pT classification, either according to the 7th edition or the 8th edition.
The UICC 8th edition staging system is considered valid for non-small cell lung cancer patients and appears to be superior in defining different prognostic groups than the 7th edition.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P1.16 - Treatment of Early Stage/Localized Disease (Not CME Accredited Session) (ID 948)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.16-61 - Intermittent Chest Tube Clamping Shortens Chest Tube Duration After Lung Cancer Surgery: An Interim Analysis of Randomized Clinical Trial (ID 11919)
16:45 - 18:00 | Author(s): Jia Wang
- Abstract
Background
Postoperative pleural drainage markedly influences the length of hospital stay and the financial costs of medical care. Our previous retrospective study proved the safety and effectiveness of chest tube clamping in the term of shortening chest tube duration. This study aims to determine if intermittent chest tube clamping could decrease chest tube duration and total drainage volume after lung cancer surgery in randomized clinical trial. This trial is registered with ClinicalTrials.gov (NCT03379350).
a9ded1e5ce5d75814730bb4caaf49419 Method
All the patients were managed with gravity drainage (water seal only, without suction) during the first 12–24 h (depending on the time of surgery completion) after surgery. Once a radiograph confirmed re-expansion of the lung on the morning of the POD1 and no air leak was detected, patients were randomly assigned to intermittent chest tube clamping as study arm or traditional chest tube management as control arm. Patients in control arm were unchangeably managed with gravity drainage. In clamping arm, the chest tube would be clamped, and the nurses would check the patient every 6 h. If the patient had no problems with compliance, the clamp was removed for 30 minutes in the morning to record the drainage volume every 24 h. The criterion for chest tube removal was drainage volume <250 mL in 24 h.
4c3880bb027f159e801041b1021e88e8 Result
Seven-two consecutive patients with operable lung cancer treated using lobectomy were randomized, all of them were eligible and evaluable. Thirty-seven and 35 patients were randomly assigned to clamping arm and control arm, respectively. There were no significant differences between two groups in terms of demographics, such of age, gender and the percentage of neoadjuvant treatment. Analyses were performed to compare drainage duration between two groups. Chest tube drainage duration was significantly shorter in clamping group than in control group (2.3±0.5 days vs. 2.7±0.9 days, p = 0.011). Total drainage volume was significantly less in clamping group than in control group (411.0±183.1 ml vs. 553.7±333.6 ml, p = 0.030). Only one patient in clamping group underwent thoracocentesis after chest tube removal due to chylothorax, which was probably caused by excess high-fat diet. No pyrexia relevant to chest tube clamping occurred. There was some degree of improvement on plasma albumin declination at discharge in clamping group over control group (7.5±2.5 g/L vs. 8.6±3.6 g/L, p = 0.119), but without a significant statistical difference.
8eea62084ca7e541d918e823422bd82e Conclusion
Intermittent postoperative chest tube clamping decreases chest tube duration and total drainage volume while maintaining patient safety. Further investigation is warranted.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P2.16 - Treatment of Early Stage/Localized Disease (Not CME Accredited Session) (ID 965)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.16-45 - Should Patients with Stage IB Non-Small Cell Lung Cancer Receive Adjuvant Chemotherapy? (ID 11211)
16:45 - 18:00 | Presenting Author(s): Jia Wang
- Abstract
Background
There’re much controversy over the necessity of adjuvant chemotherapy to stage IB non-small cell lung cancer (NSCLC) . The aim of this study is to compare the efficacy of platinum-based adjuvant chemotherapy for patients with stage IB NSCLC according to the 8th and 7th editions of the TNM staging system who underwent complete surgical resection and systemic mediastinal lymph node dissection.
a9ded1e5ce5d75814730bb4caaf49419 Method
Subjects were 569 patients who underwent pulmonary resection for primary NSCLC. Survival characteristics were compared using the 8th and 7th editions of the TNM classification.
4c3880bb027f159e801041b1021e88e8 Result
For patients in the observation and adjuvant groups, 5-year overall survival was 76.9% and 83.5%, respectively (p=0.044). In univariate analysis, lymphovascular invasion, TNM stage and performance status (PS) were risk factors for overall survival. In multivariate analysis, TNM stage (hazard ratio=5.808, 95% confidence interval 3.980-8.475, p<0.001), PS (hazard ratio=4.804, 95% confidence interval 3.113-7.413, p<0.001) and adjuvant chemotherapy (hazard ratio=1.565, 95% confidence interval 1.069-2.291, p=0.021) were risk factors for overall survival. Subset analysis showed that for patients with stage IB NSCLC, 5-year overall survival was 87.6% in the observation group (n=265) and 82.4% in the adjuvant group (p=0.021). For patients with stage IIA NSCLC, 5-year overall survival was 48.1% in the observation group and 87.7% in the adjuvant group (p<0.001). For patients with Eastern Cooperative Oncology Group (ECOG) 0, 5-year overall survival was 79.3% in the observation group and 91.6% in the adjuvant group(p=0.001). For patients with ECOG 1, 5-year overall survival was 58.6% in the observation group and 17.2% in the adjuvant group (p=0.021).
8eea62084ca7e541d918e823422bd82e Conclusion
For NSCLC patients with surgically treated, platinum-based adjuvant chemotherapy might result in worse survival than observation alone to stage IB but improve survival to stage IIA. Moreover, patients with good PS (ECOG 0) benefit fromadjuvant chemotherapy.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.16 - Treatment of Early Stage/Localized Disease (Not CME Accredited Session) (ID 982)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.16-36 - Adjuvant Chemotherapy May Improve the Outcome of Patients with Non-Small-Cell Lung Cancer with Metastasis of Intrapulmonary Lymph Nodes. (ID 11759)
12:00 - 13:30 | Author(s): Jia Wang
- Abstract
Background
Survival benefit of adjuvant chemotherapy (AC) of patients with intrapulmonary lymph node (IPLN) metastasis (level 12–14) needs investigation. We evaluated the impact of AC on patients whose metastatic nodes were limited to intrapulmonary levels after systematic dissection of N1 nodes.
a9ded1e5ce5d75814730bb4caaf49419 Method
First, 155 consective cases of lung cancer confirmed as pathologic N1 were collected and evaluated. Patients received systematic dissection of N2 and N1 nodes. For patients with IPLN metastasis, survival outcomes were compared between those receiving AC and those not receiving AC.
4c3880bb027f159e801041b1021e88e8 Result
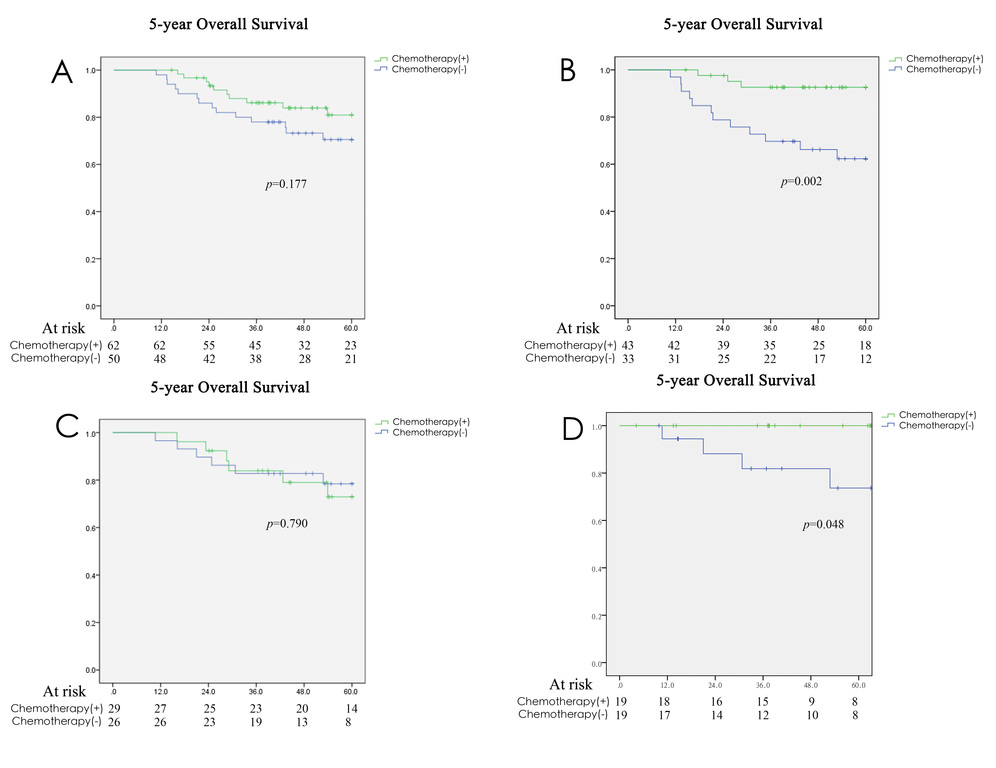
In this group, 112 cases (72.3%) had IPLN metastasis and 55 cases (35.5%) had N1 involvement limited to level 13–14 without further disease spread to higher levels. Patients with IPLN involvement had a better prognosis than that of patients with hilar–interlobar involvement. For the intrapulmonary N1 group (level 12–14-positive, level 10–11-negative or unknown, n = 112), no survival benefit was found between the AC group and non-AC group (5-year overall survival (54.6±1.6 vs. 50.4±2.4 months, p = 0.177, Figure 1A). However, 76 of 112 cases for whom harvesting of level-10 and level-11 nodes was done did not show cancer involvement in pathology reports (level 12–14-positive, level 10–11 both negative), oncologic outcome in this group was better for patients receiving AC than those not receiving AC (5-year OS: 57.3±1.5 vs. 47.1±3.2 months, p = 0.002, Figure 1B). Similarly, survival benefit of AC didn’t exist in patients with lymph node metastasis to level 13–14 (level 13–14-positive, 10-12-negative or unknown, n=55, Figure 1C), but was found in 38 patients with complete examination of N1 nodes (58.3±1.7 vs. 51.0±4.2 months, p = 0.048, Figure 1D).
8eea62084ca7e541d918e823422bd82e Conclusion
Oncologic outcome may be improved by AC for patients with involvement of N1 nodes limited to intrapulmonary levels after complete examination of N1 nodes.
6f8b794f3246b0c1e1780bb4d4d5dc53


