Virtual Library
Start Your Search
Yuqi Wang
Author of
-
+
P1.04 - Immunooncology (Not CME Accredited Session) (ID 936)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.04-34 - Study on Treatment of Stage IV Solid Tumors with Mutant Neoantigen Specific T Cells (ID 12833)
16:45 - 18:00 | Author(s): Yuqi Wang
- Abstract
Background
As an important tumor immunotherapy, the specificity and efficiency of PD1 inhibitor is not yet satisfactory. The treatment of solid tumor with mutant neoantigen specific T (Nas-T) cells developed in this study is an adoptive cell therapy which is specific for each patient. The aim is to explore the difference in safety and efficacy between Nas-T cells and PD1 inhibitors, and to evaluate the charateristic of immune repertoire (IR) as predictive biomarker.
a9ded1e5ce5d75814730bb4caaf49419 Method
A total number of 11 patients with advanced solid tumors who failed after multiline treatments were recruited. They were treated with Nas-T cells, PD1 inhibitors and BSC; other 11 patients were treated with PD1 inhibitors and BSC as control. Peripheral blood was collected at baseline and per cycle (21-28d) respectively. Multiple PCR and NGS on TCR beta chain was used to detect IR.
4c3880bb027f159e801041b1021e88e8 Result
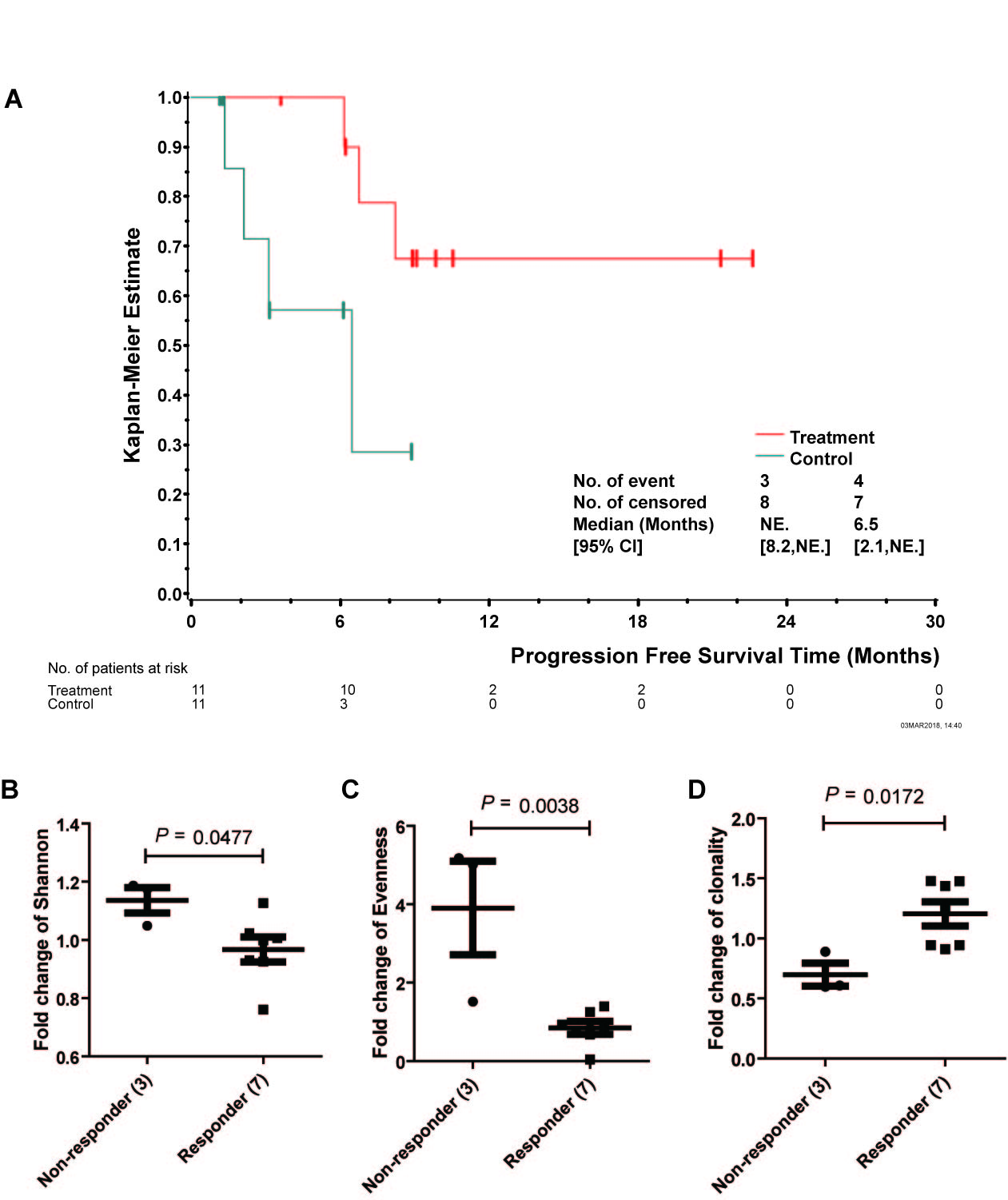
PFS of two groups had a statistical significance (P<0.05), suggesting Nas-T cells prolong patients' PFS. The safety was analyzed from routine blood urine stool test, coagulation function, liver and kidney function. There was no significant difference at baseline (P>0.05). Compared with C group, total protein and albumin in T group had a transient decrease in 3rd, 4th and 5th follow-up respectively (P<0.05), however, It can be recovered autonomously before 6th cycle.
Three indexes were examined to illuminate the diversity and clonality of IR. Compared to baseline, T cell repertoir of non-responders and responders after 1st cycle showed significant changes: Shannon 1.14 vs 0.97, P=0.048; Evenness 3.90 vs 0.85, P=0.004; Clonality 1.20 vs 0.70, P=0.017. Elevated Clonality may indicate amplification of tumor specific T cells which could recognize mutant neoantigen specifically.
8eea62084ca7e541d918e823422bd82e Conclusion
The combined immunotherapy of Nas-T cells and PD1 inhibitors is more effective than PD1 inhibitor alone in prolonging the PFS, and has a good safety. IR Clonality change shows its potential as a predictive biomarker.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.01 - Advanced NSCLC (Not CME Accredited Session) (ID 967)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.01-64 - Preliminary Data of Diverse Therapies in Patients with Advanced Non–Small-Cell Lung Cancer Harbouring RET-Rearrangement (ID 13677)
12:00 - 13:30 | Author(s): Yuqi Wang
- Abstract
Background
Activating RET-rearrangement has been discovered to play a crucial role in NSCLC tumorigenesis. However, the lack of specificity narrowed efficacy of multi-kinase inhibitors (MKIs) and the optimal treatment remains unknown. In this study, we compared chemotherapy, immunotherapy and MKIs in this group of patients.
a9ded1e5ce5d75814730bb4caaf49419 Method
We retrospectively evaluated the efficacy of these three treatments in advanced, RET-rearranged NSCLC patients between January 2013 and April 2018 at our institution. RET-rearrangements were assessed by Next-generation sequencing (NGS) or any of FISH, IHC, RT-PCR. Treatment data were collected after the patients had been diagnosed with RET-rearranged advanced NSCLC. Progression-free survival (PFS) was measured from treatment start to disease progression, all-cause mortality or last follow up. Median follow-up time was 5.1months. NGS was performed to assess somatic mutation of available samples.
4c3880bb027f159e801041b1021e88e8 Result
A total of 30 patients with RET-rearrangement were investigated in this study. After the diagnosis, 15 patients, genetic profiles confirmed by NGS, received chemotherapy (n=10), checkpoint-inhibitors (n=7) and RET targeted MKI (n=6) with evaluable response. Several patients take any two of these three treatments as different line therapies. The disease control rate of chemotherapy, immunotherapy, MKI group was 70.0%, 71.43% and 50%, respectively. While the median PFS of three groups was 2.50 months, 2.70 months, 0.30 months, respectively, which of no significance. The NGS data of 10 patients showed that RET-rearrangement co-occurred with several other genes, including TP53, NTRK, CDK4, ERBB4. A low mutation burden (mean 4.5 mutations) was observed (Figure 1).
8eea62084ca7e541d918e823422bd82e Conclusion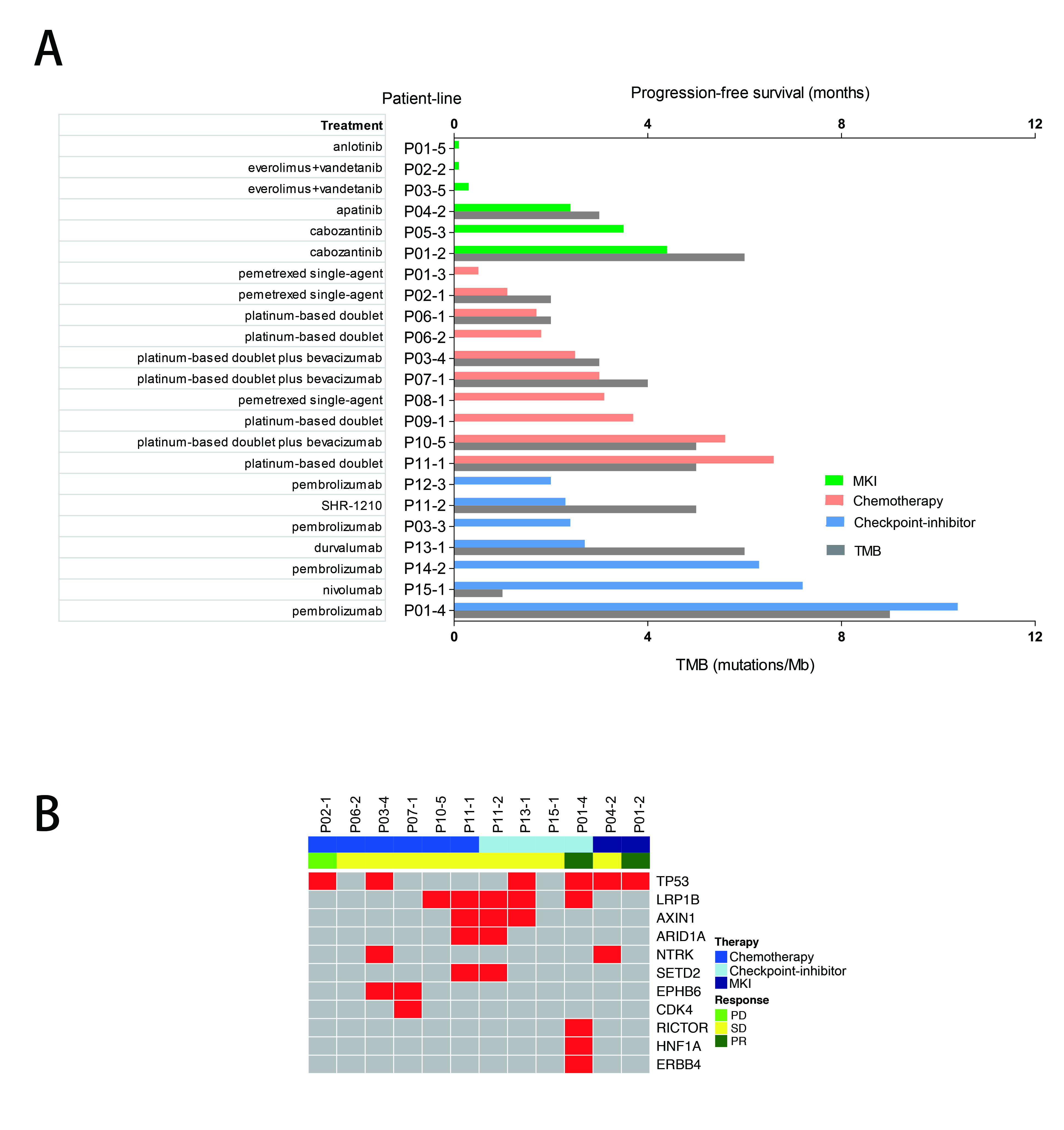
We confirmed relatively low PFS in advanced RET-rearranged NSCLC with MKIs reported in previous studies. But further investigation is warranted. Treatment with checkpoint-inhibitors seemed to encouragingly prolong PFS but a larger group of patients is needed to draw a definite conclusion.
6f8b794f3246b0c1e1780bb4d4d5dc53


