Virtual Library
Start Your Search
Winson Y Cheung
Author of
-
+
MA14 - Survivorship, Socioeconomic and End-of-Life Considerations (ID 915)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Treatment in the Real World - Support, Survivorship, Systems Research
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 10:30 - 12:00, Room 205 BD
-
+
MA14.11 - Factors Associated with Early Mortality in Non-Small Cell Lung Cancer Patients Following Systemic Anti-Cancer Treatment (ID 12970)
11:40 - 11:45 | Author(s): Winson Y Cheung
- Abstract
- Presentation
Background
To determine a 30-day mortality rate benchmark and assess factors associated with early mortality of non-small cell lung cancer (NSCLC) patients following receipt of systemic anti-cancer therapies (SACT).
a9ded1e5ce5d75814730bb4caaf49419 Method
In a 10-year population-based analysis, NSCLC patients receiving SACT in 2005-2014, with or without other treatments, and captured in the Glans-Look Lung Cancer Database, which contains demographic, clinical, pathological, treatment and outcome data were reviewed. 30-day mortality after most recent SACT cycle was calculated, and end-of life (EOL) regimen changes in the last 14 days of life were identified. Univariate analysis and multivariable logistic regression were used to identify demographic, tumor or treatment-related factors that correlated with mortality risk.
4c3880bb027f159e801041b1021e88e8 Result
1044 eligible NSCLC patients receiving at least one cycle of SACT in 2005-2014 were identified. 51% were female, 62% adenocarcinoma, 79% current/former smokers, 83% advanced stage at diagnosis, and 77% receiving palliative-intent treatment. 233 (22.3%) deaths occurred ≤ 30 days following SACT receipt, and 32 (13.7%) EOL regimen changes identified. Risk of early mortality decreased for never-smokers and those receiving SACT between 2010-2014, and increased in association with male gender, advanced disease at diagnosis, palliative-intent treatment, and use of EGFR-targeting agents. No factors were associated with a decreased risk of EOL regimen change. (Table 1). The predominant SACT-modality among those experiencing 30-day mortality was EGFR-targeting agents (54%).
8eea62084ca7e541d918e823422bd82e Conclusion
Our findings from a real-world population identify several factors which affect the risk of early mortality in NSCLC patients following SACT, and establish a 30-day mortality benchmark for Canadian NSCLC populations. Evolving SACT modalities may facilitate an increased use of SACT at EOL and associated early mortality; however, in this cohort, decreased early mortality risk in the 2010-2014 timeframe suggests concomitant evolution of decisions regarding EOL SACT and/or palliative and EOL care may be underway at our centre, but represents an area for ongoing investigation.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
P1.15 - Treatment in the Real World - Support, Survivorship, Systems Research (Not CME Accredited Session) (ID 947)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.15-34 - Treatment Patterns and Outcomes of Stage III Non-Small Cell Lung Cancer (NSCLC): Real World Evidence of How our Patients Fare (ID 14011)
16:45 - 18:00 | Author(s): Winson Y Cheung
- Abstract
Background
Most patients withstage III non-small cell lung cancer (NSCLC) develop metastases and succumb to their cancer. New treatment strategies, including concurrent chemo–RT (cCRT) followed by adjuvant immunotherapy, are improving outcomes, but need to be contextualized with real world data. In this study, we described population-based treatment patterns and outcomes for stage III NSCLC in a large Canadian province.
a9ded1e5ce5d75814730bb4caaf49419 Method
Through the provincial cancer registry, patients diagnosed with stage III NSCLC from April 1st 2010 to March 31st 2015 were identified. Using electronic medical records and administrative claims, stage III patients were merged with treatment and survival information. Patient characteristics, treatment patterns, and outcomes were analyzed.
4c3880bb027f159e801041b1021e88e8 Result
6,438 patients were diagnosed with NSCLC, including 1,151 (17.9%) with stage III disease. Median age at diagnosis was 70 years (22–94); 50.2% were male. The majority were stage IIIA (61.2%); the remainder was stage IIIB (36.4%) or unspecified (2.4%). Most patients received palliative RT (32.8%), supportive care until progression (24.8%), or palliative chemotherapy (14.8%) as initial treatments. Relatively few underwent cCRT (11.7%) or trimodality therapy (1.7%). Resection was performed on 14.8% of patients. Within the resected cohort, the majority (47.6%) did not receive further perioperative treatment, while others had surgery as part of trimodality (11.2%) or alongside perioperative chemotherapy (37.1%). Overall, the median OS (mOS) was 13.3 months (0–NR). Initial treatment strategy predicted outcomes (p< 0.05). Patients who underwent cCRT had mOS of 23.8 months (1.1–not reached [NR]). mOS for patients who initially received palliative chemotherapy or RT was 11.1 months (0.3–NR), and 6.2 (0–NR) with supportive care (Figure 1).
Figure 1: Kaplan–Meier curves for stage III NSCLC stratified by treatment class
8eea62084ca7e541d918e823422bd82e Conclusion
Treatment rates for cCRT and trimodality therapy in our cohort appear lower than expected despite evidence supporting the benefits of these strategies. Use of other treatment options was associated with poorer outcomes.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P2.01 - Advanced NSCLC (Not CME Accredited Session) (ID 950)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.01-13 - Number, Rather Than Location of Metastases, Dictates Outcome in Stage IV, M1b, Non-Small Cell Lung Cancer (ID 12799)
16:45 - 18:00 | Author(s): Winson Y Cheung
- Abstract
Background
To assess the impact of location versus number of extra-pulmonary metastatic sites (EPMS) on survival in stage IV non-small cell lung cancer (NSCLC).
a9ded1e5ce5d75814730bb4caaf49419 Method
A large scale, multi-year retrospective analysis was conducted on patients with a new diagnosis of stage IV, M1b (AJCC 7th edition) NSCLC between 1999-2013. Demographic, clinical, histopathological, treatment and outcome data was extracted from the Canadian institutional Glans-Look Lung Cancer Database. We assessed the impact of location and number of EPMS and identified correlates of overall survival using the Kaplan-Meier method and Cox regression.
4c3880bb027f159e801041b1021e88e8 Result
A total of 2,065 NSCLC patients with EPMS were identified. Median age was 67 (IQR 58-75) years, 52% were male, and 78% reported a history of smoking. 60% had one EPMS, and 40% had two or more EPMS. Among those with only one EMPS, most frequent organ involvement included bone (40%), brain (32%), liver (13%) and adrenal (10%). Median overall survival (mOS) was worst in those with liver metastasis and best in those with adrenal metastasis (2.0 vs. 5.2 months, p=0.015). However, outcomes based on organ site involvement did not retain prognostic significance in multivariable analysis after controlling for other measured confounders. Compared to patients with one EPMS, individuals with ≥ 2 EPMS experienced worse outcomes (mOS 3.9 vs 2.9 months, p<0.001), and were associated with worse prognosis in Cox regression analysis (HR 1.5, 95%CI 1.3-1.7, p<0.001). A statistically and clinically significant inverse relationship persisted between increasing number of EMPS sites and mOS. Those patients who received systemic anti-cancer therapy or surgical resection of metastatic disease (received by 25% and 3% of total cohort respectively) demonstrated the most improved mOS, regardless of number or location of EMPS (10.0 vs 2.0 months, p<0.001, and 9.0 vs 3.0 months, p<0.001, respectively).
8eea62084ca7e541d918e823422bd82e Conclusion
We conclude that number, rather than location of EPMS is a prognostic factor in patients with stage IV M1b NSCLC. A simple count of metastatic sites at diagnosis may be of clinical value in in the management and advanced care planning for patients with metastatic NSCLC. Of note, this could assist in identification of patients who would benefit from either more aggressive treatment or best supportive care, and may be an important consideration in future clinical trial design. Overall, this study reinforces the need to advance efforts to determine and mitigate the factors predisposing patients to develop metastatic disease, and develop initiatives to reduce the number of patients presenting with advanced disease.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.15 - Treatment in the Real World - Support, Survivorship, Systems Research (Not CME Accredited Session) (ID 981)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.15-30 - Treatment Patterns and Survival of Patients with Stage IV Non-Small Cell Lung Cancer (NSCLC) in the Era of Novel Therapies (ID 14042)
12:00 - 13:30 | Author(s): Winson Y Cheung
- Abstract
Background
Treatment strategies for metastatic non-small cell lung cancer (NSCLC) are evolving rapidly. Real–world evidence (RWE) of treatment patterns and outcomes can further our understanding of the impact of novel therapies. In this population-based study, we investigated treatments and outcomes for stage IV NSCLC in a large Canadian province.
a9ded1e5ce5d75814730bb4caaf49419 Method
Patients diagnosed with de novostage IV NSCLC from April 1st2010 to March 31st2015 were identified. Baseline characteristics, treatments, and outcomes were analyzed. We classified treatments targeting EGFR, EML4–ALK, and ROS1 as targeted therapy and intravenous checkpoint inhibitors as immunotherapy.
4c3880bb027f159e801041b1021e88e8 Result
A total of 6,438 patients were identified with NSCLC, of whom 3,606 (56%) had de novostage IV disease. The median age of diagnosis was 69 years (range 20–100) and 52.4% were male. The median age among those who received targeted therapy and immunotherapy were 63 (27–90) and 61 (37–72) years, respectively, and 41.8% and 61.8% were male, respectively. First line treatments were: 5.7% targeted agents (n= 204), 1% immunotherapy (n = 1), 19.5% palliative chemotherapy (n= 703), 6.8% palliative radiotherapy (n= 246), and 74.8% received supportive care only (n= 2,698). Most frequent subsequent treatments in 2L included: 30.7% targeted agents (n= 125), 1.7% immunotherapies (n= 7), 67.6% palliative chemotherapy (n= 275), 32.2% palliative radiotherapy (n= 131). Median overall survival (mOS) for the whole cohort was 3.8 months (0–not reached [NR]). MOS with targeted therapies was 18 months (1.4–NR), chemotherapy was 9.4 months (1.1–NR) and supportive care only had a mOS of 2.5 months (0–NR) (Figure 1). About 1.0% of patients (n= 34) received immunotherapy at any line.
8eea62084ca7e541d918e823422bd82e Conclusion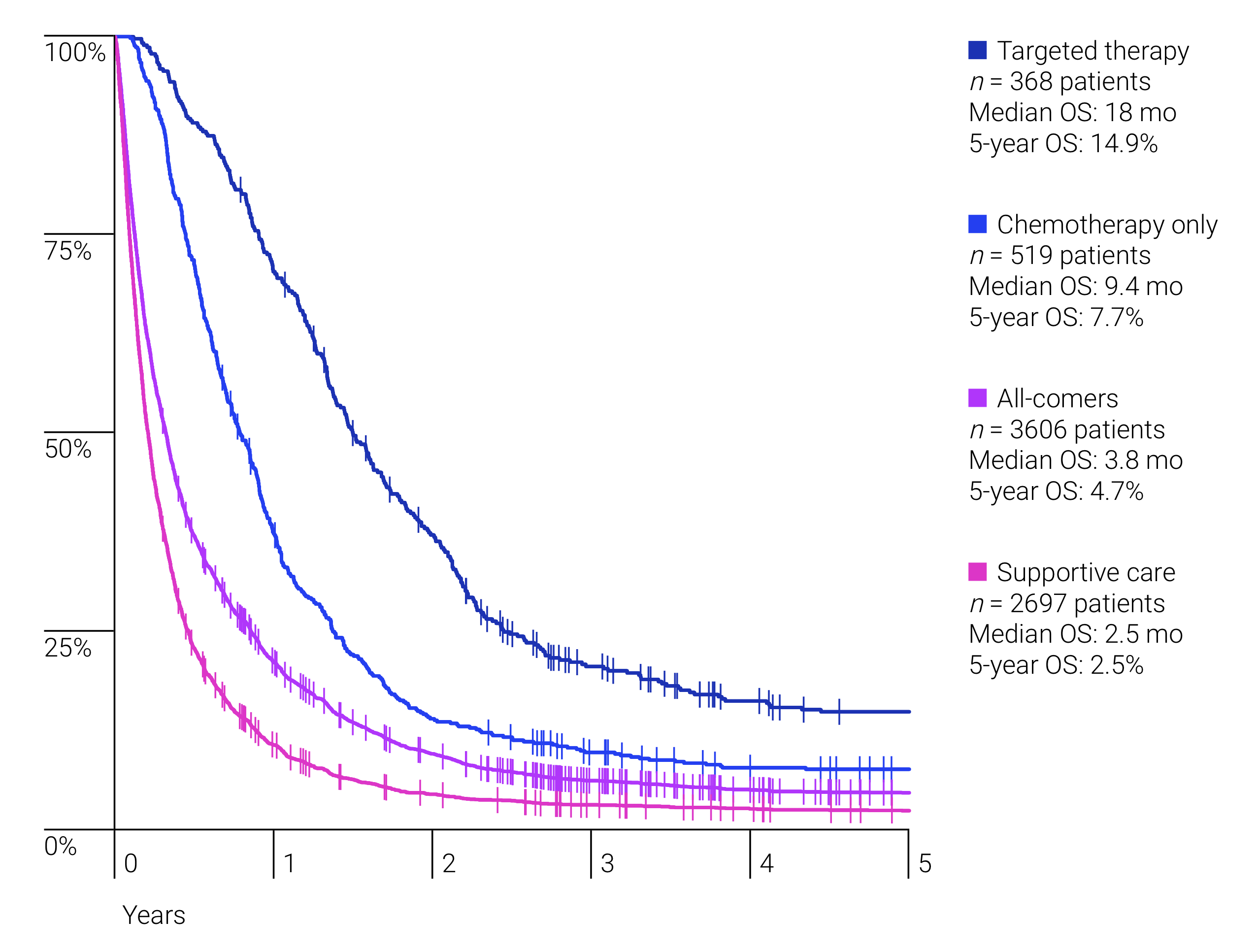
Survival benefit was dependent on type of treatment received, with a trend towards improved survival with newer agents.
6f8b794f3246b0c1e1780bb4d4d5dc53


