Virtual Library
Start Your Search
Eduard Auclin
Author of
-
+
MA08 - Clinical Trials in Brain Metastases (ID 906)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Advanced NSCLC
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 15:15 - 16:45, Room 203 BD
-
+
MA08.09 - Impact of Brain Metastases in Immune Checkpoint Inhibitors (ICI) Treated Advanced Non-Small Cell Lung Cancer (NSCLC) Patients (ID 12575)
16:10 - 16:15 | Author(s): Eduard Auclin
- Abstract
- Presentation
Background
Brain metastases (BM) are frequent in NSCLC. Unfortunately, patients with (untreated) BM are often excluded from ICI trials so that their outcome on ICI is largely unknown..
a9ded1e5ce5d75814730bb4caaf49419 Method
Retrospective data collection of all consecutive advanced ICI treated NSCLC patients in 6 centers (5 French, 1 Dutch) (nov 2012 – march 2018). Active BM was defined as non-irradiated new and/or growing lesions on brain imaging < 6 weeks before ICI start. Progression free survival (PFS), overall survival (OS) and site of progression on ICI was collected.
4c3880bb027f159e801041b1021e88e8 Result
945 patients included: 63% male, 83% WHO PS 0-1, median age 64 years, 73% non-squamous, 4% targetable driver mutations, 33% known PD-L1 (65% ≥1% expression). ICI treatment was median 2nd line (range 1-12), 94% had monotherapy PD-(L)1 inhibition. 241 patients (26%) had BM, 68% had previous cranial irradiation, 40% had active BM. BM patients were significantly younger than others (61 vs 66 years), had more adenocarcinoma (78 vs 62%), more organs involved (median 3 vs 2), a poorer PS (0-1: 76 vs 85%) and more steroids at baseline (26 vs 9%). Median follow-up: 15 months. Median (95% CI) PFS and OS without and with BM were 2 (2-3) vs 2 (1-2) months and 13 (9-16) vs 9 (7-13) months, respectively. In multivariate analysis, > 2 metastatic sites, PS ≥2 and steroids use were associated with worse PFS and OS, BM were not (table 1). In univariate analysis of BM patients, active BM were not associated with worse outcome compared to stable BM (HR PFS 0.98 (p=0.66), HR OS 0.93 (p=0.92)). Progressing BM patients had more often brain PD and a dissociated response (not specifically brain dissociated) on ICI (40 vs 12% and 13 vs 7%, respectively).
Factor PFS HR (95% CI) p-value OS HR (95% CI) p-value Age > 65 vs ≤ 65 1.02 (0.87-1.20) 0.79 1.11 (0.92-1.34) 0.29 Smoking yes vs no 0.53 (0.41-0.69) <0.001 0.81 (0.59-1.12) 0.20 Histology squamous vs adeno 1.07 (0.89-1.28) 0.78 1.24 (0.99-1.55) 0.12 Nr of organs with metastases > 2 vs ≤ 2 1.28 (1.09-1.50) 0.003 1.48 (1.22-1.80) <0.001 Immuno line > 2 vs ≤ 2 1.11 (0.94-1.30) 0.22 1.10 (0.91-1.33) 0.34 WHO PS 0-1 vs ≥2 2.14 (1.75-2.62) <0.001 3.48 (2.78-4.36) <0.001 Use of corticosteroids yes vs no 1.36 (1.10-1.69) 0.005 1.31 (1.03-1.68) 0.03 BM yes vs no 1.05 (0.88-1.26) 0.58 0.96 (0.77-1.19) 0.70
8eea62084ca7e541d918e823422bd82e Conclusion
BM, treated or active, do not negatively impact outcome on ICI although BM failure is more common in these patients.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
P1.01 - Advanced NSCLC (Not CME Accredited Session) (ID 933)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 2
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.01-18 - Immunosenescence Correlates with Progression upon PD-(L)-1 Blockade (IO) in Advanced Non-Small Cell Lung Cancer (aNSCLC) Patients. (ID 14074)
16:45 - 18:00 | Author(s): Eduard Auclin
- Abstract
Background
Immunosenescence is a progressive remodeling of immune functions with a multifactorial etiology (i.e. aging, chronic inflammation, cancer). Although a CD28-CD57+KLRG1+ phenotype on peripheral T-lymphocytes is a potential hallmark of immunosenescence, the characterization of such phenotype in IO-treated NSCLC patients and the correlation with clinical characteristics and benefit from immunotherapy are unknown.
a9ded1e5ce5d75814730bb4caaf49419 Method
A senescent immune phenotype (SIP) defined as a percentage of circulating CD8+CD28-CD57+KLRG1+ T-lymphocytes was assessed by flow cytometry (FC) on fresh blood samples from IO-treated aNSCLC patients (03/2017–04/2018). A log-rank maximization method was used to identify a SIP cut-off level and dichotomize patients accordingly. The objective was to correlate SIP with clinical characteristics and RECIST response by univariate logistic regression analysis.
4c3880bb027f159e801041b1021e88e8 Result
39 aNSCLC patients were evaluable for SIP before IO: 38% ≥ 65 years, 87% non-squamous, 38% KRAS mutated, 54% with PD-L1 expression ≥1%, 13% chemotherapy naïve. Among 30 patients evaluable for IO response, 53% had progression (PD), 27% stability (SD), 20% partial response (PR). Median PFS was 1.9 months (95% CI 1.5; 2.5). OS was not calculated due to the short follow-up [6 months (95% CI 4-11)]. SIP (% CD28-CD57+KLRG1+) median value on circulating CD8+ lymphocytes was 15.26% (min 1.87%, max 56.28%). Overall, 13 (33%) of 39 patients had >22.25% CD8+ lymphocytes with a CD28-CD57+KLRG1+ phenotype, being classified as SIP+. SIP status did not correlate with age, IO-baseline patients’ characteristics or chemotherapy exposure. Among patients evaluable for IO response, only 1 (10%) of 10 SIP+ experienced disease control (PR/SD), compared to 13 (65%) of 20 SIP- patients; similarly, PD rate was significantly higher in SIP+ compared to SIP- patients (90% vs 35%, p=0.007) (Figure).
8eea62084ca7e541d918e823422bd82e Conclusion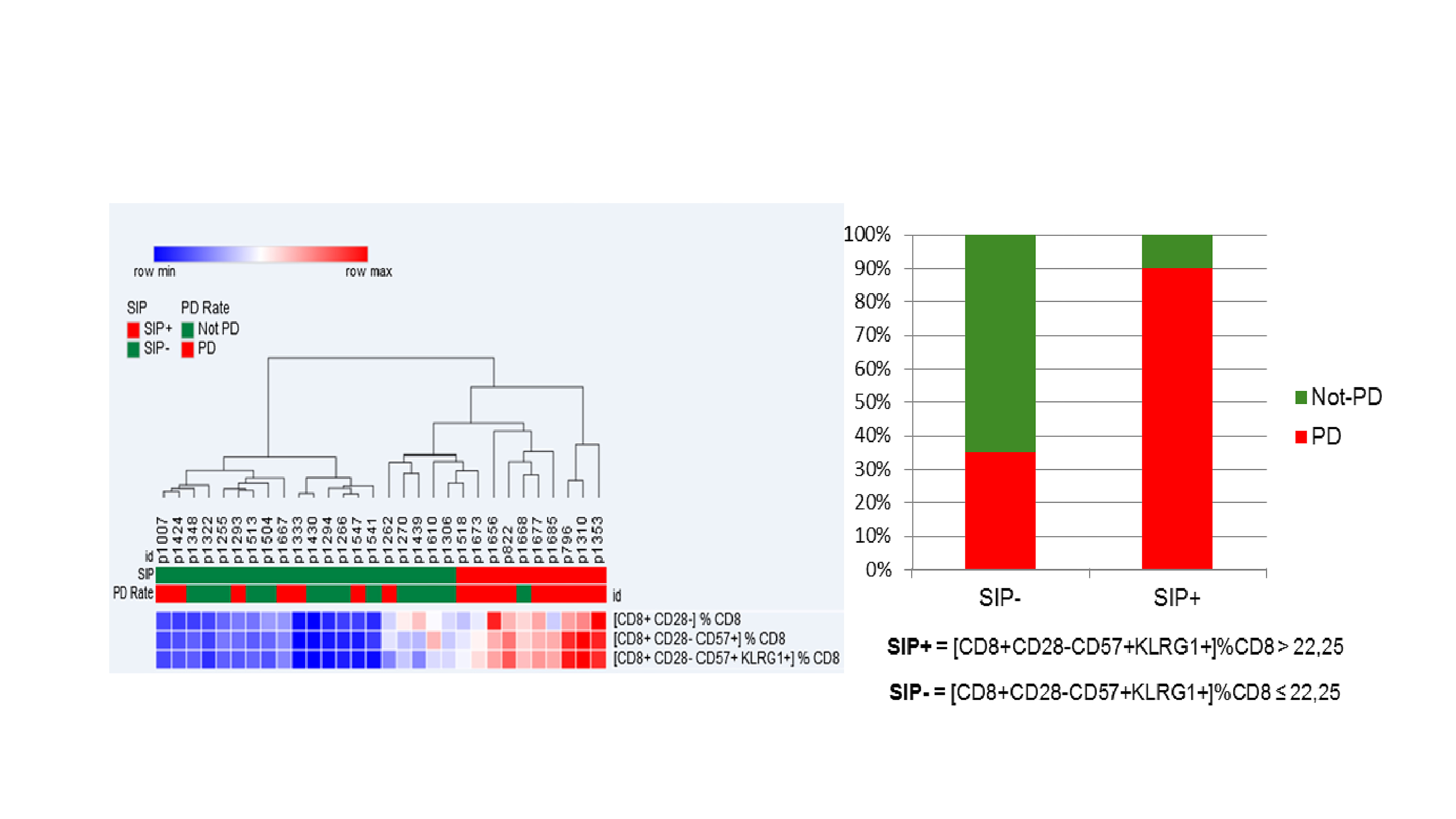
Immunosenescence, monitored by FC measurement of 3 surface molecules on circulating CD8 + lymphocytes, is observed in 33% of aNSCLC patients, is independent of age and correlates with lower IO disease control rate.
6f8b794f3246b0c1e1780bb4d4d5dc53 -
+
P1.01-19 - Efficacy of Tyrosine Kinase Inhibitors in EGFR Mutated Non-Small Cell Lung Cancer with Leptomeningeal Metastases. (ID 13820)
16:45 - 18:00 | Author(s): Eduard Auclin
- Abstract
Background
Leptomeningeal dissemination (LM) in patients with non-small cell lung carcinoma (NSCLC) is usually associated with dismal prognosis. However, survival data and optimal management of tyrosine kinase inhibitors (TKI) in EGFR-mutated (EGFRm) patients (pts) are unknown.
a9ded1e5ce5d75814730bb4caaf49419 Method
Pts with EGFRm NSCLC with LM treated in 2 institutions were included. Clinical, pathological and radiological data were retrospectively collected. We performed overall survival (OS) analysis from LM diagnosis. We assessed survival, clinical response rate (CRR) and disease control rate (DCR; stable disease > 2 months or clinical response) in patients who received a subsequent TKI after experiencing LM progression with first-line TKI.
4c3880bb027f159e801041b1021e88e8 Result
Seventy pts were included between Apr. 2003 and Feb. 2018. Median age was 54 [26-79], 60 (85%) were non-smokers, 51 (73%) female and median number of prior systemic treatments before LM diagnosis was 2 [1-7].
Median OS from LM diagnosis was 7 months (m) [95% CI 6-9], with a 1 year-OS of 29%. Pts received a median of 2 [1-6] lines of subsequent systemic therapy and 19 had additional intrathecal treatment.
At first LM progression, 40 pts received subsequent TKI treatment with a median PFS of 3m [95% CI 2-not reached]. DCR and CRR were 73% and 38%, respectively. In patients without T790M mutation (N=36), median OS was 7 months [95% CI 4-7] with 2nd-line erlotinib (N=21) and 3 months [2-17] with 2nd-line afatinib or gefitinib (N=5). Eight patients received high-dose erlotinib as 2nd-line treatment after prior erlotinib with a median OS of 3 months [1-3] and a DCR of 75%. Four patients with T790M mutation received 2nd-line osimertinib with a median OS of 10 months [6-10] and a DCR of 100%.
8eea62084ca7e541d918e823422bd82e Conclusion
Pts with LM from EGFRm NSCLC have prolonged survival with 1st generation TKI. Second-line erlotinib after LM progression is an efficient approach in T790M-negative pts. Erlotinib dose increase is a suitable strategy in erlotinib-refractory T790M-negative pts.
6f8b794f3246b0c1e1780bb4d4d5dc53


