Virtual Library
Start Your Search
Shi Yan
Author of
-
+
MA05 - Improving Outcomes in Locoregional NSCLC II (ID 901)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Treatment of Locoregional Disease - NSCLC
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 13:30 - 15:00, Room 105
-
+
MA05.11 - Radiomics Analysis Using SVM Predicts Mediastinal Lymph Nodes Status of Squamous Cell Lung Cancer by Pre-Treatment Chest CT Scan (ID 12033)
14:40 - 14:45 | Author(s): Shi Yan
- Abstract
- Presentation
Background
Assessment of mediastinal lymph nodes (N2 station) is essential in staging patients with Non-small-cell lung cancer (NSCLC), for patients with preoperative confirmed N2 status should follow neoadjuvant therapy before surgery, and occult N2 status should be avoided. There are several invasive and non-invasive exams available for preoperative N staging, like EBUS-TBNA and PET-CT scan. Chest CT scan was the basic examination of every patient, while only the length of minor axis could be used to predict lymph node involvement, and the potential value of CT might be underestimated. In this study we aimed to explore the value of radiomics analysis with machine learning in differentiating N2 from N1/N0 subjects using pre-treatment chest CT.
a9ded1e5ce5d75814730bb4caaf49419 Method
Ninety-three patients with squamous cell lung cancer, who underwent pre-treatment CT scans were included in this study. By use of Laplacian of Gaussian (LoG) filter and matrix based radiomics models (e.g. gray-level co-occurrence matrix), comprehensive radiomics features were extracted from the regions of interest which were manually delineated on primary tumors. We performed radiomics analysis using support vector machine (SVM) to test texture and heterogeneity features derived from pre-treatment CT images as indicators for the staging of lymph node metastasis, especially N2. The gold standard of N staging is confirmed pathologically after systematic mediastinal lymphadenectomy (N2 subjects=31).
4c3880bb027f159e801041b1021e88e8 Result
For the performance evaluation of single image feature, there are 16 features able to differentiate N2 subjects from others (N0 and N1) with p value <0.05. Furthermore, SVM training and classification were performed using 5-feature combinations as inputs. With feature selection, the best performance of N2 prediction is 83% accuracy with 87% sensitivity and 81% specificity.
8eea62084ca7e541d918e823422bd82e Conclusion
Radiomics analysis using SVM training can successfully predict N staging by pre-treatment chest CT scan for NSCLC patients, which could diminish the odds of occult N2 status and provide unique information preoperatively for treatment planning.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
P1.16 - Treatment of Early Stage/Localized Disease (Not CME Accredited Session) (ID 948)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.16-61 - Intermittent Chest Tube Clamping Shortens Chest Tube Duration After Lung Cancer Surgery: An Interim Analysis of Randomized Clinical Trial (ID 11919)
16:45 - 18:00 | Presenting Author(s): Shi Yan
- Abstract
Background
Postoperative pleural drainage markedly influences the length of hospital stay and the financial costs of medical care. Our previous retrospective study proved the safety and effectiveness of chest tube clamping in the term of shortening chest tube duration. This study aims to determine if intermittent chest tube clamping could decrease chest tube duration and total drainage volume after lung cancer surgery in randomized clinical trial. This trial is registered with ClinicalTrials.gov (NCT03379350).
a9ded1e5ce5d75814730bb4caaf49419 Method
All the patients were managed with gravity drainage (water seal only, without suction) during the first 12–24 h (depending on the time of surgery completion) after surgery. Once a radiograph confirmed re-expansion of the lung on the morning of the POD1 and no air leak was detected, patients were randomly assigned to intermittent chest tube clamping as study arm or traditional chest tube management as control arm. Patients in control arm were unchangeably managed with gravity drainage. In clamping arm, the chest tube would be clamped, and the nurses would check the patient every 6 h. If the patient had no problems with compliance, the clamp was removed for 30 minutes in the morning to record the drainage volume every 24 h. The criterion for chest tube removal was drainage volume <250 mL in 24 h.
4c3880bb027f159e801041b1021e88e8 Result
Seven-two consecutive patients with operable lung cancer treated using lobectomy were randomized, all of them were eligible and evaluable. Thirty-seven and 35 patients were randomly assigned to clamping arm and control arm, respectively. There were no significant differences between two groups in terms of demographics, such of age, gender and the percentage of neoadjuvant treatment. Analyses were performed to compare drainage duration between two groups. Chest tube drainage duration was significantly shorter in clamping group than in control group (2.3±0.5 days vs. 2.7±0.9 days, p = 0.011). Total drainage volume was significantly less in clamping group than in control group (411.0±183.1 ml vs. 553.7±333.6 ml, p = 0.030). Only one patient in clamping group underwent thoracocentesis after chest tube removal due to chylothorax, which was probably caused by excess high-fat diet. No pyrexia relevant to chest tube clamping occurred. There was some degree of improvement on plasma albumin declination at discharge in clamping group over control group (7.5±2.5 g/L vs. 8.6±3.6 g/L, p = 0.119), but without a significant statistical difference.
8eea62084ca7e541d918e823422bd82e Conclusion
Intermittent postoperative chest tube clamping decreases chest tube duration and total drainage volume while maintaining patient safety. Further investigation is warranted.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P2.16 - Treatment of Early Stage/Localized Disease (Not CME Accredited Session) (ID 965)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.16-45 - Should Patients with Stage IB Non-Small Cell Lung Cancer Receive Adjuvant Chemotherapy? (ID 11211)
16:45 - 18:00 | Author(s): Shi Yan
- Abstract
Background
There’re much controversy over the necessity of adjuvant chemotherapy to stage IB non-small cell lung cancer (NSCLC) . The aim of this study is to compare the efficacy of platinum-based adjuvant chemotherapy for patients with stage IB NSCLC according to the 8th and 7th editions of the TNM staging system who underwent complete surgical resection and systemic mediastinal lymph node dissection.
a9ded1e5ce5d75814730bb4caaf49419 Method
Subjects were 569 patients who underwent pulmonary resection for primary NSCLC. Survival characteristics were compared using the 8th and 7th editions of the TNM classification.
4c3880bb027f159e801041b1021e88e8 Result
For patients in the observation and adjuvant groups, 5-year overall survival was 76.9% and 83.5%, respectively (p=0.044). In univariate analysis, lymphovascular invasion, TNM stage and performance status (PS) were risk factors for overall survival. In multivariate analysis, TNM stage (hazard ratio=5.808, 95% confidence interval 3.980-8.475, p<0.001), PS (hazard ratio=4.804, 95% confidence interval 3.113-7.413, p<0.001) and adjuvant chemotherapy (hazard ratio=1.565, 95% confidence interval 1.069-2.291, p=0.021) were risk factors for overall survival. Subset analysis showed that for patients with stage IB NSCLC, 5-year overall survival was 87.6% in the observation group (n=265) and 82.4% in the adjuvant group (p=0.021). For patients with stage IIA NSCLC, 5-year overall survival was 48.1% in the observation group and 87.7% in the adjuvant group (p<0.001). For patients with Eastern Cooperative Oncology Group (ECOG) 0, 5-year overall survival was 79.3% in the observation group and 91.6% in the adjuvant group(p=0.001). For patients with ECOG 1, 5-year overall survival was 58.6% in the observation group and 17.2% in the adjuvant group (p=0.021).
8eea62084ca7e541d918e823422bd82e Conclusion
For NSCLC patients with surgically treated, platinum-based adjuvant chemotherapy might result in worse survival than observation alone to stage IB but improve survival to stage IIA. Moreover, patients with good PS (ECOG 0) benefit fromadjuvant chemotherapy.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.16 - Treatment of Early Stage/Localized Disease (Not CME Accredited Session) (ID 982)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 3
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.16-34 - The Impact of Preoperative Exercise Therapy on the Surgical Outcomes of Patients with Lung Cancer and COPD: A Systematic Review and Meta-Analysis (ID 12034)
12:00 - 13:30 | Author(s): Shi Yan
- Abstract
Background
Although isolated studies have looked at the impact of preoperative exercise on patients with lung cancer and chronic obstructive pulmonary disease (COPD), a comprehensive meta-analysis of the available data has hitherto been lacking.
a9ded1e5ce5d75814730bb4caaf49419 Method
Articles were searched from PubMed, Embase, and Cochrane library, with the following criteria: lung cancer patients with or without COPD; undergoing resection; receiving preoperative exercise training. Key outcomes were analyzed using meta-analysis.
4c3880bb027f159e801041b1021e88e8 Result
Seven studies containing 404 participants were included. Patients receiving preoperative exercise training had a lower incidence of postoperative pulmonary complications (PPCs) (Odds Ratio (OR) 0.35, 95% Confidence Interval (CI) 0.21 to 0.59) and shorter length of hospital stay (Standard Mean Difference −1.02 days, 95% CI −1.31 to −0.74 days). Exceptionally, incidence of pneumonia remained unchanged. Patients with COPD could not obviously benefit from exercise training to reduce PPCs(OR 0.44, 95% CI 0.18 to 1.08)but still might achieve faster recovery. No significant difference in pulmonary function was observed between the two groups. However, 6-minutes walking distance and VO2 peak were significantly improved after exercise training.
8eea62084ca7e541d918e823422bd82e Conclusion
Preoperative exercise training might not reduce PPCs for COPD patients undergoing lung cancer resection, but still facilitate faster recovery. Muscle capacity was strengthened after rehabilitation, which emphasized the possible mechanism of the protocol design.
6f8b794f3246b0c1e1780bb4d4d5dc53 -
+
P3.16-35 - Stair Climbing Exercise May Ameliorate Pulmonary Function Impairment in Patients at One Month After Lung Cancer Resection (ID 12136)
12:00 - 13:30 | Author(s): Shi Yan
- Abstract
Background
Surgical resection remains the primary treatment for patients with localized non-small cell lung cancer (NSCLC). Despite the possibility of a cure, lung resection is associated with an immediate pulmonary function impairment.
Stair-climbing test as a reliable indicator of pulmonary function, is often performed preoperatively to select patients. It also has been reported that stair-climbing yielding greater values of VO2 is a more stressful exercise than cycle ergometry. The benefits of this intervention in postoperative patients remain unclear. Thus, this study aimed to evaluate the effects of performance at the postoperative symptom-limited stair climbing exercise on pulmonary function.
a9ded1e5ce5d75814730bb4caaf49419 Method
We retrospectively analyzed 36 consecutive NSCLC patients undergoing video-assisted thoracoscopic surgery lobectomy and systematic mediastinal lymphadenectomy from November 2017 to January 2018. In the postoperative pulmonary rehabilitation program, all patients were suggested to perform symptom-limited stair climbing exercise in addition to routine physiotherapy (walking, incentive spirometry, breathing) from the first day after surgery. Patients were encouraged to climb gradually to the maximum number of floors at a pace of their own choice, and to stop in case of exhaustion, insufferable pain, limiting dyspnea or leg fatigue. A nursing professional was indispensable for the management of chest drains and supervision of any symptoms. Heart rate, pulse oxygen saturation were continuously measured using a portable pulse oximeter. Stair climbing exercise was performed at least twice a day during and after hospital stay. According to their performance of the exercise, patients could be divided into two groups. Stair climbing group completed the exercise training as planned, while routine physiotherapy group was reluctant to stair climbing exercise except for routine physiotherapy. Pulmonary functions were performed on all patients preoperatively and at one month postoperatively.
4c3880bb027f159e801041b1021e88e8 Result
Totally, 25 patients (15 in stair climbing group and 10 in routine physiotherapy group) were included in the final analysis. The average preoperative and postoperative FEV1 for patients in two groups were 2.69±0.83 L vs. 3.08±0.72 L (p=0.244) and 2.08±0.72 L vs. 2.23±0.60 L (p=0.592), respectively. The difference in FEV1 decline between stair climbing group and routine physiotherapy group was significant (0.61±0.26 L vs. 0.84 ± 0.23 L, p=0.032).
8eea62084ca7e541d918e823422bd82e Conclusion
This study suggested that symptom-limited stair climbing as a more stressful exercise performed postoperatively in patients may ameliorate pulmonary function impairment at one month after lung resection. Prospective randomized controlled trials are therefore warranted.
6f8b794f3246b0c1e1780bb4d4d5dc53 -
+
P3.16-36 - Adjuvant Chemotherapy May Improve the Outcome of Patients with Non-Small-Cell Lung Cancer with Metastasis of Intrapulmonary Lymph Nodes. (ID 11759)
12:00 - 13:30 | Author(s): Shi Yan
- Abstract
Background
Survival benefit of adjuvant chemotherapy (AC) of patients with intrapulmonary lymph node (IPLN) metastasis (level 12–14) needs investigation. We evaluated the impact of AC on patients whose metastatic nodes were limited to intrapulmonary levels after systematic dissection of N1 nodes.
a9ded1e5ce5d75814730bb4caaf49419 Method
First, 155 consective cases of lung cancer confirmed as pathologic N1 were collected and evaluated. Patients received systematic dissection of N2 and N1 nodes. For patients with IPLN metastasis, survival outcomes were compared between those receiving AC and those not receiving AC.
4c3880bb027f159e801041b1021e88e8 Result
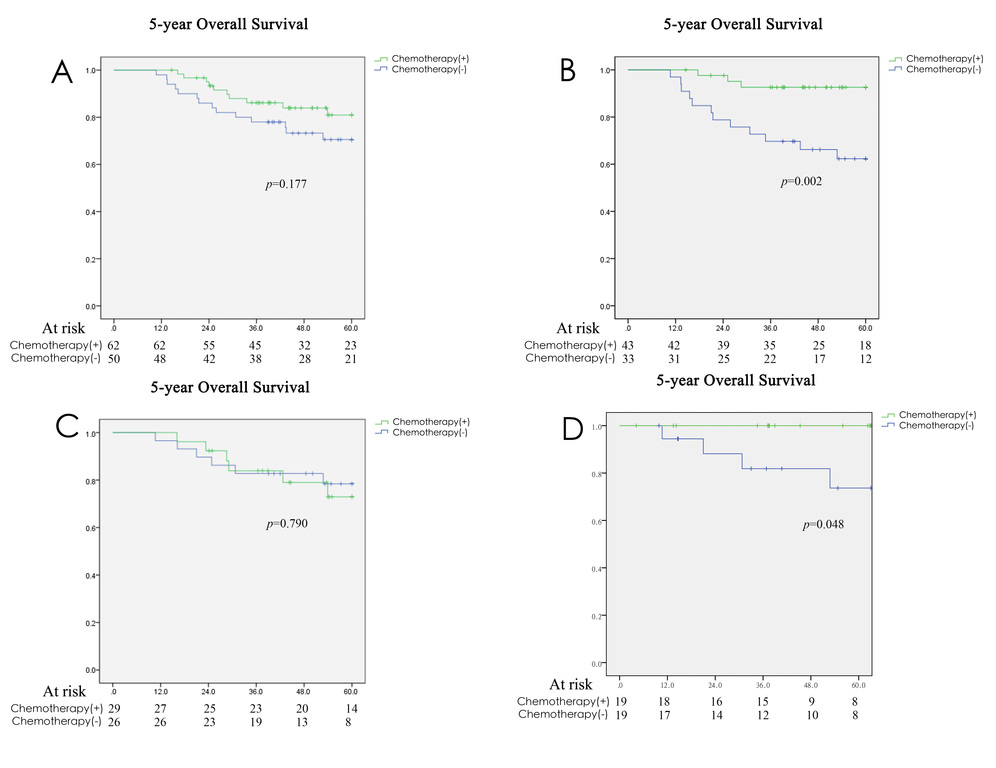
In this group, 112 cases (72.3%) had IPLN metastasis and 55 cases (35.5%) had N1 involvement limited to level 13–14 without further disease spread to higher levels. Patients with IPLN involvement had a better prognosis than that of patients with hilar–interlobar involvement. For the intrapulmonary N1 group (level 12–14-positive, level 10–11-negative or unknown, n = 112), no survival benefit was found between the AC group and non-AC group (5-year overall survival (54.6±1.6 vs. 50.4±2.4 months, p = 0.177, Figure 1A). However, 76 of 112 cases for whom harvesting of level-10 and level-11 nodes was done did not show cancer involvement in pathology reports (level 12–14-positive, level 10–11 both negative), oncologic outcome in this group was better for patients receiving AC than those not receiving AC (5-year OS: 57.3±1.5 vs. 47.1±3.2 months, p = 0.002, Figure 1B). Similarly, survival benefit of AC didn’t exist in patients with lymph node metastasis to level 13–14 (level 13–14-positive, 10-12-negative or unknown, n=55, Figure 1C), but was found in 38 patients with complete examination of N1 nodes (58.3±1.7 vs. 51.0±4.2 months, p = 0.048, Figure 1D).
8eea62084ca7e541d918e823422bd82e Conclusion
Oncologic outcome may be improved by AC for patients with involvement of N1 nodes limited to intrapulmonary levels after complete examination of N1 nodes.
6f8b794f3246b0c1e1780bb4d4d5dc53


