Virtual Library
Start Your Search
Jianjun Zhang
Author of
-
+
MA06 - PDL1, TMB and DNA Repair (ID 903)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Biology
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 13:30 - 15:00, Room 206 AC
-
+
MA06.02 - Prospective Immunogenomic Profiling of Non-Small Cell Lung Cancer: Genomic and Immune Profiling Updates from Project ICON (ID 13523)
13:35 - 13:40 | Author(s): Jianjun Zhang
- Abstract
- Presentation
Background
Our previous work has demonstrated that higher level of genomic complexity is associated with more heterogeneous neoantigen repertoire, suppressed T cell repertoire and postsurgical relapse in localized non-small cell lung cancers (NSCLC) highlighting the complex interaction of tumor molecular and immune landscape and their impact on cancer biology and patient survival. We launched the ICON Project (Immune Genomic Profiling of NSCLC) to prospectively delineate the molecular and immune landscape of early stage NSCLC and their impact on patient survival through a multidisciplinary approach. Here we report the updated genomic and immune analyses.
a9ded1e5ce5d75814730bb4caaf49419 Method
Surgical specimens from stage I-III NSCLC were subjected to whole-exome and RNA sequencing for mutational analysis, in silico neoantigen prediction and gene expression analysis as well as T cell receptor sequencing, cytometry by time-of-flight and multiplex immunofluorescence staining.
4c3880bb027f159e801041b1021e88e8 Result
From 2016-2018, 127 patients were accrued and 50 surgical samples have undergone WES, RNAseq, TCR sequencing and immune phenotyping. Median age is 66 yrs (range: 39-86), 52% (26/50) were female and 76% (38/50) former smokers. 76% (38/50) are non-squamous carcinomas and 24% (12/50) squamous cell carcinomas. 34% have stage I disease (17/50), 30% stage II (15/50), 34% stage III (17/50) and 2% stage IV (1/50). The majority of patients had upfront surgery (45/50; 90%). With median follow-up of 19 months, 15 patients have relapsed. Median tumor mutational burden is 7.8mut/Mb and predicted neoantigen burden was 10/sample (range: 0-250). Predicted neoantigen burden is significantly correlated with tumor mutational burden (r=0.41, p=0.002). The most commonly mutated genes are TP53, KRAS, CDKN2A, PIK3CA, EGFR, BRAF, GRIN2A and ATM. C->A transversions and C->T transitions were the most common mutational subtypes. PD-1 expression and regulatory T-cell (CD4+/FoxP3+) infiltration are significantly increased in tumor tissue compared to normal tissue (p=0.003 and p=0.02 respectively), while CD3, CD8, granzyme B and CD45RO are decreased in tumor tissue compared to normal lung.
8eea62084ca7e541d918e823422bd82e Conclusion
NSCLC tumors have an immunosuppressive microenvironment compared to tumor adjacent normal lung tissues. Clinical data will be adequate to conduct genomic and immune profiling comparisons across different clinical subgroups. Mutational and neoantigen profiling are consistent with previously reported studies and correlations between molecular and immune landscapes and its impact on patient survival are ongoing.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
MA19 - Genomic Markers of IO Response (ID 922)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Immunooncology
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 15:15 - 16:45, Room 201 BD
-
+
MA19.10 - Impact of STK11/LKB1 Genomic Alterations on Clinical Outcomes with Chemo-Immunotherapy in Non-Squamous NSCLC (ID 14295)
16:15 - 16:20 | Author(s): Jianjun Zhang
- Abstract
- Presentation
Background
Chemo-immunotherapy with pemetrexed/carboplatin/pembrolizumab represents a standard of care for the first-line treatment of patients with metastatic non-squamous NSCLC, irrespective of tumor cell PD-L1 expression. Genomic determinants of response to chemo-immunotherapy in NSCLC have not been reported thus far. We previously identified STK11/LKB1 alterations as a major genomic driver of de novo resistance to PD-1/PD-L1 inhibitor monotherapy in NSCLC (Skoulidis et al., Cancer Discovery, 2018). Here, we examine the impact of STK11/LKB1 mutations on clinical outcomes with chemo-immunotherapy with pemetrexed/carboplatin/pembrolizumab.
a9ded1e5ce5d75814730bb4caaf49419 Method
Patients with metastatic non-squamous NSCLC that received at least 1 cycle of pemetrexed/carboplatin/pembrolizumab at MD Anderson Cancer Center, were alive for ≥14 days thereafter and had available next generation sequencing- based comprehensive tumor genomic profiling were eligible. Response assessment was based on RECIST1.1. PD-L1 expression on tumor cells was evaluated using the FDA-approved 22C3 pharmDx assay. All patients consented to collection of clinical and molecular data as part of the GEMINI protocol.
4c3880bb027f159e801041b1021e88e8 Result
Among 49 eligible patients (median age 61 years, 51% female, 96% adenocarcinoma histology, 34.7% KRAS-mutant) the objective response rate to pemetrexed/carboplatin/pembrolizumab was 51% (25/49) for the overall population. The disease control rate (PR+SD≥ 6 months) differed significantly between STK11/LKB1-mutant and STK11/LKB1-wild-type tumors (31.3% vs 72.7%, P=0.011, two-tailed Fisher’s exact test). The objective response rate was 31.3% for STK11/LKB1-mutant and 60.6% for STK11/LKB1 wild-type tumors (P=0.07, two-tailed Fisher’s exact test). 37.5% (6/16) of STK11/LKB1-mutant tumors exhibited progressive disease as best overall response to chemo-immunotherapy compared with 6.1% (2/33) STK11/LKB1-wild-type tumors (P=0.01, two-tailed Fisher’s exact test). Patients bearing STK11/LKB1-mutant tumors exhibited shorter progression-free survival with chemo-immunotherapy (median PFS 4.4 months vs 11.0 months, P=0.039, log-rank test). STK11/LKB1-mutant tumors were less likely to be positive for PD-L1 expression (PD-L1 TPS ≥ 1%), although the difference did not reach statistical significance (43.8% vs 72%, P=0.1, two-tailed Fisher’s exact test).
8eea62084ca7e541d918e823422bd82e Conclusion
STK11/LKB1 genomic alterations are associated with inferior clinical outcomes with chemo-immunotherapy in non-squamous NSCLC, with response rates comparable to those previously reported for platinum doublet chemotherapy alone. Assessment of STK11/LKB1 status may help refine treatment approaches in non-squamous NSCLC.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
MA23 - Early Stage Lung Cancer: Present and Future (ID 926)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Treatment of Early Stage/Localized Disease
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 10:30 - 12:00, Room 105
-
+
MA23.02 - Circulating Tumor DNA Analysis with a Novel Variant Classifier for Recurrence Detection in Resected, Early-Stage Lung Cancer (ID 13498)
10:35 - 10:40 | Author(s): Jianjun Zhang
- Abstract
- Presentation
Background
ctDNA is a blood-based biomarker with promising potential in lung cancer for minimal residual disease (MRD) assessment and early detection of recurrence. However, data regarding feasibility are limited, especially for stage I-II disease.
a9ded1e5ce5d75814730bb4caaf49419 Method
We performed longitudinal plasma ctDNA profiling of early-stage lung cancer patients (pts) that underwent resection at MD Anderson Cancer Center from Apr 2016 to Jan 2017. Plasma ctDNA was analyzed from pre-operative and multiple post-operative time points until disease recurrence. ctDNA profiling was performed using a 30kb Digital Sequencing panel (Guardant Health) covering SNVs in 21 genes and indels in 9 genes that are commonly present in lung cancer. ctDNA profiles from ~30,000 lung cancer pts were used to train a classifier to exclude non-tumor related mutations.
4c3880bb027f159e801041b1021e88e8 Result
A total of 40 pts were included in this analysis, comprised of the first 17 pts with recurrence in the longitudinal study and 23 consecutive pts without recurrence. This cohort was primarily stage I and II (15 [38%], 16 [40%]). Histology included adenocarcinoma (29 [73%]), SCC (6 [15%]), and SCLC (2 [5%]). 58% had adjuvant therapy. Median follow-up was 17.7 (3.4 – 24.5) months and median time to recurrence was 7.1 (3.4 – 16.5) months in this selected cohort. At least one ctDNA alteration was detected in 55% (21/38) of pts with evaluable pre-op samples and in 22% (8/37) of pts at 4 weeks post-op. Presence of ctDNA at 4 weeks post-op heralded eventual recurrence with 43% sensitivity and 91% specificity (75% PPV, 73% NPV) and was significantly associated with worse recurrence free survival (p=0.022, HR 6.52; 95% CI 1.3 – 32.6), while also accounting for stage. In the absence of the variant classifier, an additional 7/37 pts had non-tumor alterations detected at 4 weeks post-op with a recurrence sensitivity and specificity of 57.1% and 69.6%. ctDNA was identified in 76% (13/17) of pts prior to or at the time of recurrence. The median interval between ctDNA detection and radiographic recurrence was 91 days.
8eea62084ca7e541d918e823422bd82e Conclusion
Detection of post-op ctDNA, as early as 4 weeks after resection of early-stage lung cancer, is associated with significantly increased risk of recurrence. Accurate detection of ctDNA in this MRD setting is enabled by a highly sensitive sequencing platform that incorporates a novel variant classifier to enhance clinical specificity.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA03 - Advances in Lung Cancer Pathology (ID 897)
- Event: WCLC 2018
- Type: Oral Abstract Session
- Track: Pathology
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 10:30 - 12:00, Room 205 BD
-
+
OA03.05 - Characterization of the Immunologic Intra-Tumor Heterogeneity in Early Stages of Non-Small Cell Lung Cancer by Multiplex Immunofluorescence (ID 13334)
11:15 - 11:25 | Author(s): Jianjun Zhang
- Abstract
- Presentation
Background
Recurrence of non-small cell lung carcinoma (NSCLC) is associated with genetic and epigenetic intra-tumor heterogeneity (ITH). The interaction between malignant cells, stromal cells, and tumor-associated immune-cells (TAICs), such as T-cell lymphocytes (TCLs) and tumor-associated macrophages (TAMs), is important for progression of NSCLC and the characterization of the immunologic ITH might be relevant to predict recurrence in surgically treated patients at early stages of NSCLC. The aim of this study was to characterize the immunologic ITH of primary NSCLC tumors at early stages using image analysis and multiplex immunofluorescence (mIF) approaches.
a9ded1e5ce5d75814730bb4caaf49419 Method
Eight cases of stage IA and 8 cases of stage IB surgically resected NSCLC (11 adenocarcinomas, ADCs; and 5 squamous-cell carcinomas, SCCs) with a history of early recurrence were selected for this preliminary analysis. FFPE blocks were obtained and consecutive sections were stained with two panels of mIF for immune profiling, panel 1: pan-cytokeratin (AE1/AE3), PD-L1, PD-1, CD3, CD8, and CD68; panel 2: AE1/AE3, CD3, CD8, granzyme-B (GB), CD45RO, and FOXP3. Three not adjacent, intra-tumor regions (3mm2 each) per case were randomly selected after gridding the whole tumor section. A total of 41 intra-tumor regions were scanned by Vectra multispectral-microscope and analyzed using InForm-software. TAICs were quantified in epithelial and stromal compartments from each intra-tumor region. G-Cross AUC (area under the curve) was computed for specific intervals of distances between TAICs and malignant cells. Median distance between TAICs and malignant cells within each region was calculated.
4c3880bb027f159e801041b1021e88e8 Result
The median density of TCLs and TAMs were 1527 cells/mm2 and 635 cells/mm2, respectively, without significant differences between histologic subtypes. TCLs were predominantly concentered in stromal compartment (median, 2222 cells/mm2) compared with epithelial compartment (median, 332 cells/mm2). Percentage and density of TCLs and TAMs varied 4 and 8 times, respectively, between cases and regions. Non-cytotoxic T-cells and inactive cytotoxic T-cells were the most prevalent phenotypes. Higher density of TAMs and antigen-experienced TCLs were observed in stage IB than stage IA.
8eea62084ca7e541d918e823422bd82e Conclusion
Characterization of immunologic ITH of NSCLC is able by mIF and image analysis with FFPE tumor tissue. There is variability of TAICs densities between regions from the same tumor and different subpopulations were observed. TAMs and exhausted T-cells were more prominent in stage IB (tumor >3cm) suggesting these cells may play an important role in recurrence. Ongoing studies with a larger cohort and comparison with non-recurrent surgically treated patients are warranted. Supported by CPRITRP160668 and UTLungSPORE grants
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
P1.04 - Immunooncology (Not CME Accredited Session) (ID 936)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.04-22 - CD73 Immunohistochemical Expression in Malignant Cells and Correlation with Immune Infiltrate in Non-Small Cell Lung Carcinoma (NSCLC). (ID 11859)
16:45 - 18:00 | Author(s): Jianjun Zhang
- Abstract
Background
CD73 is potential novel target for lung cancer immunotherapy involved in the adenosine pathway that induces tumor microenvironment immunosuppression. We investigated the immunohistochemical (IHC) expression of CD73 in a large cohort of NSCLC and correlated with tumor’s clinical, pathological, molecular and immune cells infiltration data.
a9ded1e5ce5d75814730bb4caaf49419 Method
We examined 175 surgically resected stages I-III formalin-fixed and paraffin-embedded NSCLC tumors tissue microarrays, including 107 adenocarcinomas (ADC) and 68 squamous cell carcinomas (SqCC). For IHC, we used the anti-CD73 antibody (clone D7F9A, Cell Signaling Technology) and evaluated membrane (basolateral and luminal) expression in malignant cells. In a subset of cases, CD73 IHC expression was correlated with data available on: a) CD73 gene mRNA expression (Illumina arrays; n=91); b) EGFR and KRAS mutation status and mutational load (whole exome sequencing; n=104); and, c) density of tumor associated immune cells infiltration (CD3, CD4, CD8, CD68, CD45RO, CD57, FOXP3, and granzyme B) and immune checkpoints expression (PD-L1, PD-1, ICOS, TIM-3, IDO-1, B7-H3, B7-H4, VISTA and OX40) assessed by IHC and image analysis (n=172).
4c3880bb027f159e801041b1021e88e8 Result
ADC showed higher CD73 IHC expression than SqCC (P<0.0001). Pathological stage I ADCs showed higher CD73 expression than higher tumor stages (P=0.0419). Using any level of CD73 expression (>1%) CD73 was expressed in 73% and 40% of ADCs and SqCs, respectively. High expression (>50% of malignant cells) was detected in 35% of ADCs and 20% of SqCC. No other significant correlations with clinical-pathological variables, including patients’ outcome were found. Interestingly, ADCs with EGFR (P=0.04) and KRAS (P=0.02) mutation expressed higher CD73 levels than wild-type tumors. In ADC, CD73 IHC expression correlated significantly with the density of immune T CD3+, CD4+, CD8+, CD45RO+ and FOXP3+ cells, as well as macrophages CD68+ cells in tumors (r values range: 0.22-0.45; P values range: 0.001-0.02). Overall, we did not find significant correlations between CD73 immunostaining and the IHC expression of the immune checkpoints examined. CD73 IHC expression correlated positively with mRNA CD73 gene expression levels in all NSCLCs (r=0.6; P<0.0001), ADCs (r=0.6; P<0.0001), and SqCCs (r=0.49, P<0.0001) histology
8eea62084ca7e541d918e823422bd82e Conclusion
We identified that CD73 protein expresses in a subset of resected NSCLCs, being significantly higher in adenocarcinoma histology. In this histology type, CD73 correlates with immune T cells and macrophages infiltration, and notably, with tumor’s EGFR and KRAS mutation. Our data suggest that CD73 is a potential target for NSCLC, particularly for adenocarcinoma histology (Supported by grants CPRIT RP160668 and UT Lung SPORE).
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P1.13 - Targeted Therapy (Not CME Accredited Session) (ID 945)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.13-37 - Clinical Evaluation of Plasma-Based (cfDNA) Genomic Profiling in Over 1,000 Patients with Advanced Non-Small Cell Lung Cancer (ID 14332)
16:45 - 18:00 | Author(s): Jianjun Zhang
- Abstract
Background
Tumor genomic information from a simple blood collection revealing actionable mutation can improve clinical outcome without the need for an invasive tissue biopsy. We report on the clinical utility of a cell-free DNA (cfDNA) next generation sequencing (NGS) blood test in our patients with non-small cell lung cancers (NSCLC) and the outcome of treatments with targeted therapies based on the reported mutations.
a9ded1e5ce5d75814730bb4caaf49419 Method
From May 2015 to February 2017, 1078 blood samples from 1011 consecutive patients with a diagnosis of NSCLC were collected and analyzed using next-generation sequencing of cfDNA with a panel of up to 70 cancer-related genes at a CLIA-certified lab (Guardant360, Guardant Health, Redwood City, CA) with reported sensitivity of 0.02% mutant allele fraction with high specificity (> 99.9999%) (CCR 2018 (17):3831). Patients in this retrospective study received targeted therapy as indicated by cfDNA molecular profiling. Tumor response was evaluated by RECIST V1.1 and standard clinical evaluation.
4c3880bb027f159e801041b1021e88e8 Result
From 1011 patients, 1078 cfDNA tests sent (additional follow-up tests: 1 in 64 patients and 2 in 3 patients). In 223/1011 (22%) patients had cfDNA report with at least 1 targetable mutations; with 48/223 (22%) patients meeting criteria for this retrospective review. Study population were 31 female:17 male, median age of 63 years (ranged:31-94). The rationale for the blood test included: insufficient tissue or not available (32%), addition to tissue molecular analysis (17%), alternative to tissue biopsy(10%), on-going treatment evaluation/resistance (41%). Mutations included:EGFR T790M (15), EGFR exon 19del (12), EGFR L858R (9), EGFR exon 20 insertion (4), EGFR others (1), ALK gene fusions (5) and MET exon 14 skipping (2). The median line of therapy was 2(ranged:1-7) with 28 patients receiving TKI as 1st line of therapy based on cfDNA mutations. With targeted treatments based on ctDNA results, the responses (RECIST V1.1) were: CR(3), PR(26), SD(14) and PD(4); median PFS was 8.5 months (ranged:1-26mos) for the overall population with 4 patients still receiving targeted therapy. Median PFS was 9.5 months (ranged:1-20 months) for those receiving TKI as 1st line.
8eea62084ca7e541d918e823422bd82e Conclusion
This is the largest analysis of response rates with cfDNA directed therapy in advanced NSCLC and demonstrates positive clinical outcomes in patients treated with targeted therapy based on plasma identified biomarkers.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P2.01 - Advanced NSCLC (Not CME Accredited Session) (ID 950)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.01-87 - Profiling the Symptom Burden of Patients with Metastatic NSCLC Receiving Either Chemotherapy or Targeted Therapy: Real-World Data (ID 13348)
16:45 - 18:00 | Author(s): Jianjun Zhang
- Abstract
Background
An understanding of the patient experience is lacking for newly developed cancer treatments, such as targeted therapies. We profiled the patient-reported outcome (PRO)-measured symptom burden experienced by patients with metastatic non-small cell lung cancer (mNSCLC) during 6 months of conventional chemotherapy or targeted therapy.
a9ded1e5ce5d75814730bb4caaf49419 Method
During 2017, patients with mNSCLC at a single institution were recruited and completed the MD Anderson Symptom Inventory lung cancer module (MDASI-LC) at clinic visits. The MDASI-LC assesses the severity of 13 core and 3 lung-cancer-specific symptoms and 6 interference items on 0‒10 scales (0=no symptom or interference, 10=worst imaginable symptom or complete interference). Descriptive statistics for MDASI-LC scores over 6 months of treatment were summarized. Symptom trajectories for the chemotherapy patients versus the targeted-therapy patients were compared via linear mixed-effects models.
4c3880bb027f159e801041b1021e88e8 Result
Of 65 patients receiving chemotherapy and 27 receiving targeted therapy, the targeted-therapy group had more women (74% vs. 49%, P=0.029) and younger patients (57.6±12.2 vs. 64.2±9.9 years, P=0.012). Before treatment, both groups reported similar symptom burden, although sadness was worse in the targeted-therapy group (2.4±1.6 vs. 0.8±1.5, P=0.021). During the first 60 days of treatment, patients receiving chemotherapy reported significant increase in pain (estimate (est)=0.03, P=0.037) and interference with walking (est=0.04, P=0.025). Compared with those receiving chemotherapy, patients receiving targeted therapy experienced significantly less severe pain (est=‒1.17, P=0.024), fatigue (est=‒1.16, P=0.019), and shortness of breath (est=‒1.23, P=0.028) and less interference with walking (est=‒1.23, P=0.042) (figure 1). More severe dry mouth was reported by patients undergoing targeted therapy (est=1.17, P=0.027).
8eea62084ca7e541d918e823422bd82e Conclusion
This real-world data demonstrates that, compared with conventional chemotherapy, targeted therapy correlates with less impairment of physiological condition and functioning in patients with mNSCLC. Additional follow up will confirm and expand these findings about the patient experience relative to treatment response.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P2.04 - Immunooncology (Not CME Accredited Session) (ID 953)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.04-09 - Driver Mutations are Associated with Distinct Patterns of Response to Immune Checkpoint Blockade in Non-Small Cell Lung Cancer (ID 13362)
16:45 - 18:00 | Author(s): Jianjun Zhang
- Abstract
Background
Immune checkpoint blockade (IO) has demonstrated durable clinical benefit in metastatic non-small cell lung cancer (NSCLC). Tumors with driver mutations such as EGFR exon 19 and 21 mutations and ALK translocation tend to have low response rates to IO. However, IO response in NSCLC patients with rare driver mutations, such as EGFR exon 20 (~2%), HER-2 (~2%) and BRAF (~3%), representing approximately 7% of lung adenocarcinomas, has been poorly addressed.
a9ded1e5ce5d75814730bb4caaf49419 Method
We queried GEMINI (MD Anderson Lung Cancer Moon Shot funded database for prospective collection of clinical information on NSCLC) for patients with mutations in EGFR exon 19, 20, 21, HER-2 and BRAF treated with PD-1/PD-L1 checkpoint inhibitors. We assessed progression-free survival (PFS), overall response rate (ORR) and overall survival (OS) in each molecular group.
4c3880bb027f159e801041b1021e88e8 Result
Between 2014-2018, 108 patients with classic EGFR mutations (exon 19 del + exon 21 L858R, n=37), EGFR exon 20 mutations (n=36; no T790M included), HER-2 mutations (n=22) and BRAF mutations (n=13; V600E: 3pts; non-V600E: 10pts) had been treated with PD-1/PD-L1 inhibitors. EGFR exon 20 mutants and BRAF mutants demonstrated significantly higher PFS (EGFR exon 20: HR 0.4, p<0.001; BRAF: HR 0.2, p<0.001), higher disease control rate at 6 and 12 months as well as higher ORR when compared to classic EGFR mutants (Table). These differences remained significant in multivariate analysis after adjusting for age, smoking, PD-L1 status, radiation prior to treatment initiation, treatment with concurrent agents and prior treatment with TKIs. HER-2 mutants had similar PFS compared to EGFR classic mutants (HR 0.8, p=0.35) (Table).
8eea62084ca7e541d918e823422bd82e Conclusion
EGFR exon 20 and BRAF mutations are associated with superior outcome from PD-1/PD-L1 checkpoint inhibitors compared to classic EGFR and HER-2 mutations. Further studies on co-mutational status and tumor mutation burden in these molecularly-defined groups are ongoing to address potential underlying mechanisms associated with these findings.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.01 - Advanced NSCLC (Not CME Accredited Session) (ID 967)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 2
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.01-109 - Real-World Patient-Reported Outcome Assessment of Patients with Metastatic Non-Small Cell Lung Cancer (ID 12213)
12:00 - 13:30 | Author(s): Jianjun Zhang
- Abstract
Background
Patient-Reported Outcomes (PROs) provide information on patient treatment experience. We have established a real-world Advanced Non-Small Cell Lung Holistic Registry (ANCHoR) to understand how the advent of immunotherapy impacts treatment choice, clinical outcomes, and PROs of metastatic non-small cell lung cancer (mNSCLC). The aim of this analysis is to report early results of baseline symptom status and quality of life among mNSCLC patients using the MD Anderson Symptom Inventory lung cancer module (MDASI-LC) and EuroQol-5D 5-level version (EQ-5D-5L).
a9ded1e5ce5d75814730bb4caaf49419 Method
During 2017, patients with mNSCLC at a single institution were enrolled in ANCHoR and completed the PRO questionnaires at clinic visits. MDASI-LC consists of thirteen core and three lung cancer-specific symptom severity questions, and six interference items rated on 0-10 scales (0 = no symptom or interference, 10 = worst imaginable symptom or complete interference). EQ-5D-5L captures five health state dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression rated on a five-level scale (1= no problems, 5= extreme problems). A single visual analogue scale (VAS) on EQ-5D-5L records patient self-rated health between ”best imaginable” (100) and “worst imaginable” (0) health state. Descriptive statistics for PRO scores at baseline are summarized.
4c3880bb027f159e801041b1021e88e8 Result
Forty-two patients completed baseline PROs before the start of therapy. Mean patient age was 63 years and 45% were males. For MDASI-LC, the mean scores for the core symptom, lung cancer-specific symptom, and interference subscales at baseline were 2.2 (standard deviation [SD] = 2.80), 2.1 (SD = 2.80), and 2.8 (SD = 3.10), respectively. Fatigue was the most severe symptom reported at baseline (mean = 4.1, SD = 3.01), followed by shortness of breath (mean = 3.2, SD = 2.81) and pain (mean = 3.19, SD = 3.00). The highest percentages of patients reporting moderate to severe symptom levels (score of ≥5) were 38% for fatigue, 33% for pain, 31% for drowsiness, 29% for shortness of breath and disturbed sleep, and 26% coughing. For EQ-5D-5L, 91% of patient reported problems with self-care, 81% with mobility, 48% with usual activity and anxiety, and 33% with pain. Mean EQ-5D VAS was 73.9 (SD = 18.2).
8eea62084ca7e541d918e823422bd82e Conclusion
Prior to the start of treatment, fatigue, pain, drowsiness, disturbed sleep, and coughing were the most common symptoms with fatigue, shortness of breath, and pain being the most severe. Additional follow up will confirm and expand these findings and will also allow us to examine change in PROs after first-line treatment is administered.
6f8b794f3246b0c1e1780bb4d4d5dc53 -
+
P3.01-91 - Computing the Impact of Immunotherapy on the Non-Small Cell Lung Cancer (NSCLC) Therapeutic Landscape (ID 12209)
12:00 - 13:30 | Author(s): Jianjun Zhang
- Abstract
Background
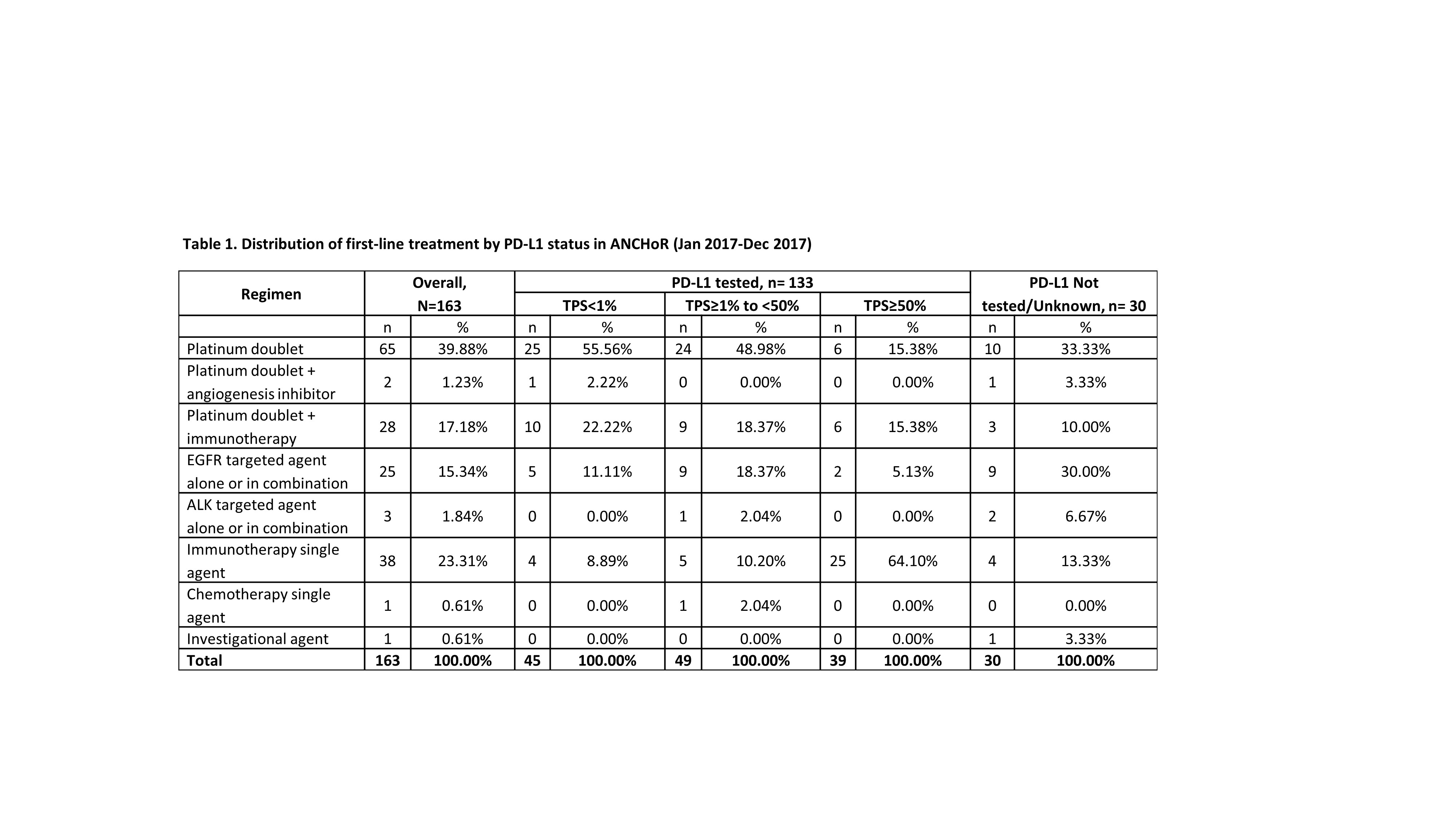
The Advanced Non-Small Lung Holistic Registry (ANCHoR) is established to examine the real-world impact of immunotherapy on choice of treatment, clinical outcomes, and patient reported outcomes of patients with Stage IV NSCLC.
a9ded1e5ce5d75814730bb4caaf49419 Method
Stage IV NSCLC patients diagnosed or initiating treatment at MD Anderson from January 1, 2017 are enrolled in the ongoing ANCHoR study. Their demographic, clinicopathological, molecular, and treatment data were populated in a prospective database. Treatment patterns by line and PD-L1 status were summarized in this interim analysis.
4c3880bb027f159e801041b1021e88e8 Result
At the time of data cut off (Dec 31, 2017) 182 patients were enrolled in the registry, of which 150 were tested for PD-L1. Number of patients initiating first-, second-, and third-line treatment were 163, 42 and 7, respectively. Of the 30 patients not tested for PD-L1, 10 did not have enough tissue and 8 had actionable mutations.
8eea62084ca7e541d918e823422bd82e Conclusion
The emergence of immunotherapy has had a dramatic impact on the first-line treatment of patient with advanced NSCLC. As of December, 2017 up to 41% of patient received immunotherapy either singly (23%) or in combination with chemotherapy. Only 40% of the patients now receive chemotherapy alone. There has been dramatic decrease in the use of chemotherapy with an anti-angiogenesis agent (1.23%). In our dataset 16% of the patients were eligible for targeted therapy as initial treatment.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.09 - Pathology (Not CME Accredited Session) (ID 975)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.09-27 - Histopathologic Parameters Define Features of Treatment Response to Neoadjuvant Chemotherapy in Non-Small Cell Lung Cancer (ID 14257)
12:00 - 13:30 | Author(s): Jianjun Zhang
- Abstract
Background
Previous studies indicate that neoadjuvant chemotherapy improves survival in patients with loco-regionally advanced non-small cell lung cancer (NSCLC). The amount of residual viable tumor has been associated with long-term overall survival. This histopathologic measure has potential to become a standard method for evaluation of the effectiveness of neoadjuvant therapy regimens. However, adequate comparison of chemotherapy-treated and untreated lung cancers is lacking. We analyzed histopathologic characteristics of resected NSCLC with and without prior neoadjuvant chemotherapy.
a9ded1e5ce5d75814730bb4caaf49419 Method
Histopathologic assessment was performed of specimens obtained from patients enrolled on the immunogenomic lung cancer study (ICON), which integrates clinical, pathologic, immune, genomic and outcome data from surgically resected NSCLC. Cases included material from 10 patients who underwent neoadjuvant chemotherapy and 10 patients treated with primary surgery (adenocarcinoma, n=5; squamous cell carcinoma, n=5; for each cohort). Hematoxylin and eosin-stained tumor sections (mean, 6; range, 3-10) were evaluated and semiquantitatively scored for parameters commonly attributed to treatment response. The percentage of viable tumor was estimated by comparison to the proportion of fibrosis and necrosis on each slide. Additional parameters analyzed included the presence of inflammation, tertiary lymphoid structures (TLS), macrophages, lymphovascular invasion (LVI), cholesterol clefts, giant cells and neovascularization (score 0-3). For each patient, the results for all slides were averaged to determine a mean value. P values were calculated using the Mann-Whitney test.
4c3880bb027f159e801041b1021e88e8 Result
All histopathologic parameters typically associated with treatment response could also be identified in untreated specimens, albeit in different proportions. Compared to the untreated cohort, samples after chemotherapy were characterized by lower proportion of viable tumor (42.4% vs 67.7%, p=0.04) and higher degrees of fibrosis (46.6% vs 26.6%, p=0.08), and necrosis (11.0 % vs 5.6%, p=0.35). Among the additional parameters, similar scores were seen for inflammation (1.54 vs 1.46, p=0.60), TLS (1.00 vs 0.80, p=0.47), LVI (0.16 vs 0.23, p=0.62), and neovascularization (both 0) while macrophages (0.94 vs 0.12, p=0.20), cholesterol clefts (0.92 vs 0.13, p= 0.03) and giant cells (0.80 vs 0.40, p=0.17) were more common among the neoadjuvant cohort.
8eea62084ca7e541d918e823422bd82e Conclusion
Histopathologic variables commonly associated with chemotherapy treatment response can also be identified in treatment naïve lung cancers. However, the amount of viable tumor, fibrosis and cholesterol clefts are parameters strongly associated with neoadjuvant therapy. These results highlight the importance of assessing the type and extent of treatment response. Analysis of larger patient cohorts will reveal potential prognostic value in primary tumors, chemotherapy-treated, and eventually immunotherapy-treated tumors.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.15 - Treatment in the Real World - Support, Survivorship, Systems Research (Not CME Accredited Session) (ID 981)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.15-29 - Defining the Symptom Burden of Non-Small Cell Lung Cancer (ID 12361)
12:00 - 13:30 | Author(s): Jianjun Zhang
- Abstract
Background
Symptom burden is disease and treatment symptom severity and its impact on daily functioning. Symptom monitoring has demonstrated improved cancer patient outcomes, including quality of life, resource utilization, ability to continue treatment, and survival. The use of disease-specific patient-reported outcomes (PRO) measures facilitates individualized symptom monitoring and management. The purpose of this study was to describe symptom experience from the patient perspective and identify key symptoms for a PRO measure of non-small cell lung cancer (NSCLC) symptom burden.
a9ded1e5ce5d75814730bb4caaf49419 Method
Patients with NSCLC described their symptom experience in single qualitative interviews. Content analysis was used to define the content for a PRO measure of NSCLC symptom burden.
4c3880bb027f159e801041b1021e88e8 Result
Mean age of the 40 patients interviewed was 66.1 years (standard deviation = 10.9); 60.0% were male, 77.5% were white, and 56.4% had stage IV disease. Content analysis found a total of 32 symptoms, 6 reported by ≥ 20% of participants (see Table 1). Symptoms varied based on treatment modality (chemotherapy versus radiation therapy), but not stage of disease. Numbness or tingling and sore mouth were described only by patients who had received chemotherapy. Patients volunteered ways in which symptoms impacted daily activities and relationships.
Table 1. Patient quotes from qualitative interviews describing the 6 most common symptoms (reported by ≥ 20% of participants) Symptom Participant Quote Shortness of breath “The heaviness, it’s like a—wow, I don’t know how to explain it—like a rock and hard to breathe sometimes, just shortness of breath. Of course, the more I try to walk, or whatever, I’m more short of breath.”
‒ 67-year-old femaleCough “I had a real bad cough. I think I actually even broke a couple of ribs coughing so much.”
‒ 52-year-old male
Distress “Terrifying. There’s no ways about it. You know, it’s a terrifying experience, especially when it’s dropped in your lap and you have to deal with it. You go through a lot physically and mentally.”
‒ 67-year-old maleFatigue “I'm more tired. I take a lot of naps where I never had been a nap person. Before I had all my energy, and I was doing lots of things, and now I'm wore out. I wake up, and I'm wore out.”
‒ 53-year-old malePain “You keep trying to move it to make it feel better and no matter where you put it, it doesn’t feel any better … most of the time it will bother me after I get out of bed in the morning for a while. And then if I go try to take a nap, I’ll go ahead and take something for pain because I can’t lay there and—I just keep moving it and moving it and nothing helps.”
- 68-year-old maleConstipation “I didn’t have a bowel movement. I had always taken the stool softeners because they told me to do that. And I kept thinking, “Well, it’s going to work. It’s going to work.” Finally, I was in so much pain that I couldn’t stand anymore, so I went to the hospital … and they ended up physically removing, which was horrible.”
‒ 68-year-old female
8eea62084ca7e541d918e823422bd82e Conclusion
Patients with NSCLC experience numerous symptoms related to disease and treatment. Shortness of breath, cough, distress, fatigue, pain, and constipation were commonly reported symptoms, suggesting that clinicians should routinely and proactively monitor the presence and severity of these symptoms in NSCLC clinical care. In patients receiving chemotherapy, attention to specific treatment-related symptoms, including symptoms of neuropathy and sore mouth, is needed. While stage of disease does not produce unique symptoms, the severity of the symptoms may possibly vary by stage of disease. Clinicians should also be aware that symptoms result in interference with daily activities, relationships, life plans, treatment adherence, and mood.
6f8b794f3246b0c1e1780bb4d4d5dc53


