Virtual Library
Start Your Search
Emanuela Taioli
Author of
-
+
MA01 - Early Stage Lung Cancer: Questions and Controversies (ID 894)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Treatment of Early Stage/Localized Disease
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 10:30 - 12:00, Room 202 BD
-
+
MA01.05 - Opioids and Sleep Medication Use After Surgery for Early Stage Lung Cancer: A SEER-Medicare Analysis (ID 12961)
11:00 - 11:05 | Author(s): Emanuela Taioli
- Abstract
- Presentation
Background
More than 50% of patients undergoing surgery for early stage lung cancer experience persistent post-operative pain, which can prevent their returning to normal daily activities and cause disruptions in sleep. Whether Video-Assisted Thoracoscopic Surgery (VATS), a minimally invasive surgical technique, reduces long-term opioid and sleep medication use compared to traditional open surgery has not yet been established.
a9ded1e5ce5d75814730bb4caaf49419 Method
The Surveillance, Epidemiology and End Results data linked to Medicare data (SEER-Medicare) database was queried to identify patients with stage I primary non-small cell lung cancer (NSCLC) who had VATS or open resection between 2007 to 2013, and had no record of opioid medication in the 30 days before surgery. Long-term opioid and sleep medication use were defined as having fulfilled one or more prescriptions in the first 90 days after surgery as well another prescription in the 90-180 days post-surgery. Logistic regression was used to investigate the associations between surgical type and long-term opioid and sleep medication use. Models were adjusted for relevant clinical and socioeconomic covariates.
4c3880bb027f159e801041b1021e88e8 Result
There were 3,900 NSCLC patients included in this analysis; 1,987 (51.0%) VATS and 1,913 (49.0%) open surgery patients; 15.5% of patients had a record of opioid use and 9.7% of sleep medication use long-term postoperatively.
In the adjusted model, patients were less likely to use opioids long-term if they had VATS (ORadj 0.69, 95% CI: 0.57-0.84), were older (ORadj 0.96, 95% CI: 0.94-0.98), diagnosed in a later year (ORadj 0.86, 95% CI: 0.82-0.90), and had higher income (ORadj 0.77, 95% CI: 0.60-0.99). Long-term opioid use was more likely in those with a higher comorbidity score (ORadj 1.10 , 95% CI: 1.05-1.16), large cell histology (ORadj 1.88, 95% CI: 1.17-3.00), using sleep medication before surgery (ORadj 1.72, 95% CI: 1.28-2.32) and with a previous psychiatric condition (ORadj 1.64, 95% CI: 1.28-2.09).
After adjustment, only those with a previous psychiatric condition (ORadj 1.95, 95% CI: 1.40-2.71) and previous sleep medication use (ORadj 37.36, 95% CI: 27.92-50.00) were more likely to use sleep medications long-term; no significant difference were observed with type of surgery (ORadj 1.01, 95% CI: 0.76-1.33).
8eea62084ca7e541d918e823422bd82e Conclusion
Patients who were not previous opioid users became long-term opioid users after surgery. VATS might offer NSCLC patients a better quality of life than open surgery, and therefore minimize the risk of longer-term opioid use.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
MA12 - Mesothelioma Surgery and Novel Targets for Prognosis and Therapy (ID 913)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Mesothelioma
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 10:30 - 12:00, Room 202 BD
-
+
MA12.02 - Quality of Life Following Pleurectomy Decortication and Extrapleural Pneumonectomy for Pleural Malignant Mesothelioma (ID 12983)
10:35 - 10:40 | Author(s): Emanuela Taioli
- Abstract
- Presentation
Background
Few studies have focused on quality of life (QoL) after treatment of malignant pleural mesothelioma (MPM). Questions remain as to which surgical procedure, extrapleural pneumonectomy (EPP) or pleurectomy (P/D), is most effective and results in better outcomes for survival and involves fewer complications. A comprehensive review was conducted on MPM patients to assess differences in QoL following P/D and EPP.
a9ded1e5ce5d75814730bb4caaf49419 Method
Original research studies on QoL after mesothelioma surgery were identified through May 2018: 17 articles, 14 datasets encompassing 659 patients, were retrieved. Measures of lung function (FEV, FVC) and EORTC QLQ-C30 were compared 6 months following surgery with preoperative values.
4c3880bb027f159e801041b1021e88e8 Result
QoL data was available for 102 EPP patients and 432 P/D patients. Two studies directly compared QoL between the two techniques. While QoL was still compromised 6 months following surgery, P/D patients fared better than EPP patients across all QoL measures. Physical function, social function, global health and dyspnea were higher at follow-up for PD than for EPP, while other indicators such as pain and cough were similar. FEV and FVC were higher at follow-up for P/D compared to EPP, although only one study reported FEV and FVC following EPP.
8eea62084ca7e541d918e823422bd82e Conclusion
QoL is better for patients undergoing P/D compared to EPP for an extended period following surgery. Given the need for multimodality therapy and the aggressive nature of MPM, QoL outcomes should be strongly considered when choosing type of surgery for MPM.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
P1.16 - Treatment of Early Stage/Localized Disease (Not CME Accredited Session) (ID 948)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.16-57 - Outcomes of Pulmonary Resection in Elderly Non-Small Cell Lung Cancer Patient (ID 11989)
16:45 - 18:00 | Author(s): Emanuela Taioli
- Abstract
Background
Because of increasing in life span and more than third-fourth of lung cancer patients being age > 60-65 years old, appropriate treatment of old lung cancer patients has become an important issue. The aim of this study is to evaluate the short and long-term surgical outcomes in elderly patients, and to identify prognostic factors of overall mortality.
a9ded1e5ce5d75814730bb4caaf49419 Method
Medical records of patients with non-small cell lung cancer (NSCLC) who underwent pulmonary resection at Chiang Mai University Hospital from January 2002 through December 2016 were retrospectively reviewed. Patients were divided into two groups; age less than 70 years (non-elderly group) and 70 years or more (elderly group). Primary outcome was major post-operative complications and in-hospital death; secondary outcome was long-term survival. Logistic regression and cox proportional hazard model were used to analyze data.
4c3880bb027f159e801041b1021e88e8 Result
This study included 583 patients; 167 in elderly group, and 416 in non-elderly group. Patients in elderly group were more likely to have government insurance, be active smoker, and have a diagnosis of COPD, an abnormal ECG, to undergo a sublobar resection, lymph node sampling, and no chemotherapy treatment than those in the non-elderly group. There were no differences in term of in-hospital mortality, composite post-operative complications, and overall mortality. At multivariable analysis, the composite post-operative complications in the elderly group was not statistically different from the non-elderly group (Adjusted odd ratios = 0.52, 95% CI=0.21-1.28), however the elderly group was more likely to die (HRadj)=2.44, 95%CI=1.26-4.74). Adverse prognostic factors for overall mortality in elderly patients were a poorly differentiated tumor (HRadj=3.53, 95%CI=1.45-8.61) and the presence with perineural invasion (HRadj=3.95, 95%CI=1.14-13.77)
Table 1 prognostic factors for overall mortality of elderly NSCLC patients after pulmonary resection
Variables
Hazard Ratio
95% CI
p-value
Male vs Female
1.43
0.62-3.26
0.401
Smoking amount
≥20 pack-year
0.91
0.45-1.82
0.783
Stage of cancer
Stage I
1.00
Reference
Stage II
0.76
0.36-1.57
0.452
Stage III
2.18
0.92-5.16
0.077
Stage IV
1.70
0.53-5.46
0.373
Grading of cell differentiation
Well
1.00
Reference
Moderately
0.80
0.39-1.67
0.558
Poorly
3.53
1.45-8.61
0.006
Undifferentiated
1.72
0.41-7.31
0.462
Intratumoral lymphatic invasion
2.73
0.99-7.52
0.052
Intratumoral vascular invasion
1.76
0.91-3.39
0.092
Perineural invasion
3.95
1.14-13.77
0.031
SLND versus SLNS
0.51
0.24-1.10
0.084
Chemotherapy
No chemotherapy
1.00
Reference
Adjuvant or induction therapy
0.69
0.33-1.46
0.330
1st-line treatment
0.76
0.15-3.80
0.734
Sublobar resection versus lobectomy
1.78
0.65-4.90
0.261
8eea62084ca7e541d918e823422bd82e Conclusion
Surgery in elderly NSCLC is a safe procedure. Patients presenting with perineural invasion and poorly differentiated tumor should be further considered for possible adjuvant treatment.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P2.06 - Mesothelioma (Not CME Accredited Session) (ID 955)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.06-35 - Pleurectomy Decortication Versus Extrapleural Pneumonectomy in Malignant Pleural Mesothelioma: SPARCS Data (ID 13265)
16:45 - 18:00 | Author(s): Emanuela Taioli
- Abstract
Background
Malignant pleural mesothelioma (MPM) is a rare but grave cancer with poor survival. To date, the debate on the surgery of choice in patients with operable MPM is still ongoing. We evaluated surgery-related mortality and post-operative complications among patients treated with Extrapleural Pneumonectomy (EPP) vs Pleurectomy Decortication (P/D) in the New York Statewide Planning and Research Cooperative System (SPARCS) database.
a9ded1e5ce5d75814730bb4caaf49419 Method
SPARCS is an all payer claim database for the State of New York. Data of inpatient stays (1995-2012) were used to extract 3826 unique patients with a diagnosis of MPM (ICD-9-CM: 163 identifying 233 patients treated with EPP (ICD-9-CM codes: 325, 3259) and 267 patients treated with P/D (ICD-9-CM codes: 345, 3451). We used propensity score methods using a logistic regression model matching patients on the following variables: age, race, the presence or absence of comorbidities, type of insurance and type of admission (using 1:1 matching with absolute difference in scores of 0.08).
4c3880bb027f159e801041b1021e88e8 Result
There was no difference in the proportion of males between EPP (76.2%) and P/D (80.9%). EPP patients were younger (mean age 60.8 vs 68.6 years), significantly more likely to be white (94.0% vs 85.2%), privately insured (56.6% vs 29.9%) and admitted for an elective procedure (97.9% vs 66.8%) than P/D patients. There were significantly more comorbidities in the EPP group (95.3% vs 85.9%). The in-hospital mortality in the matched patients groups comparing EPP and P/D was higher but not significant [ORadj: 2.82 (95% CI: 0.70-11.38)]. The odds of having postoperative complications was 1.22 (95% CI: 0.68-2.20) when comparing EPP and P/D. Supraventricular arrhythmia as postoperative complication was significantly more frequent after EPP compared to P/D (ORadj: 2.73; 95% CI: 1.14-6.50).
8eea62084ca7e541d918e823422bd82e Conclusion
The analysis showed a tendency towards higher odds of in-hospital mortality for EPP versus P/D however not statistically significant. While the odds of postoperative complications were not significantly different between EPP and P/D patients, the odds of supraventricular arrhythmia as postoperative complication were 2.7 times higher after EPP versus P/D. P/D, a less invasive surgical approach, may provide a better option when technically feasible for MPM patients.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P2.15 - Treatment in the Real World - Support, Survivorship, Systems Research (Not CME Accredited Session) (ID 964)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.15-28 - Effect of Insurance Types on Tumor Recurrence and Overall Survival in Resectable Non-Small Lung Cancer Patients in Northern Thailand (ID 12375)
16:45 - 18:00 | Author(s): Emanuela Taioli
- Abstract
Background
The effect of insurance types on tumor recurrence and overall survival in resectable non-small cell lung cancer in northern Thailand have never been reported. The aim of this study is to identify the association between Thailand’s insurance types and long-term outcomes of treatment.
a9ded1e5ce5d75814730bb4caaf49419 Method
Medical records of patients with non-small cell lung cancer (NSCLC) who underwent pulmonary resection at Chiang Mai University Hospital from January 2002 through December 2016 were retrospectively reviewed. Patients were divided into two groups; patients with National Health Security insurance (NHSI) and patients with Government/State Enterprise insurance or private insurance (GEI). Patient characteristics, pathologic findings and long-term outcomes were assessed. Primary outcome was overall survival; secondary outcome was tumor recurrence. Multivariable cox’s regression analysis were used to analyze data.
4c3880bb027f159e801041b1021e88e8 Result
This study included 583 patients; 344 with NHSI and 239 with GEI. Patients with NHSI were more likely to be active smokers, lower % predicted FEV1, present with higher stage tumor, having moderately and poorly differentiated tumor, present with tumor necrosis, and undergo open surgical approach than those with GEI. There were no differences between the two groups in term of lymph node dissection, chemotherapy and post-operative complications. At multivariable analysis, tumor recurrence in patients with GEI was not statistically different from what observed in patients with NHSI (adjusted hazard ratio (HRadj)=1.03, 95% CI=0.51-2.11), however patients with NHSI was more likely to die (HRadj=2.45, 95%CI=1.11-5.42).
8eea62084ca7e541d918e823422bd82e Conclusion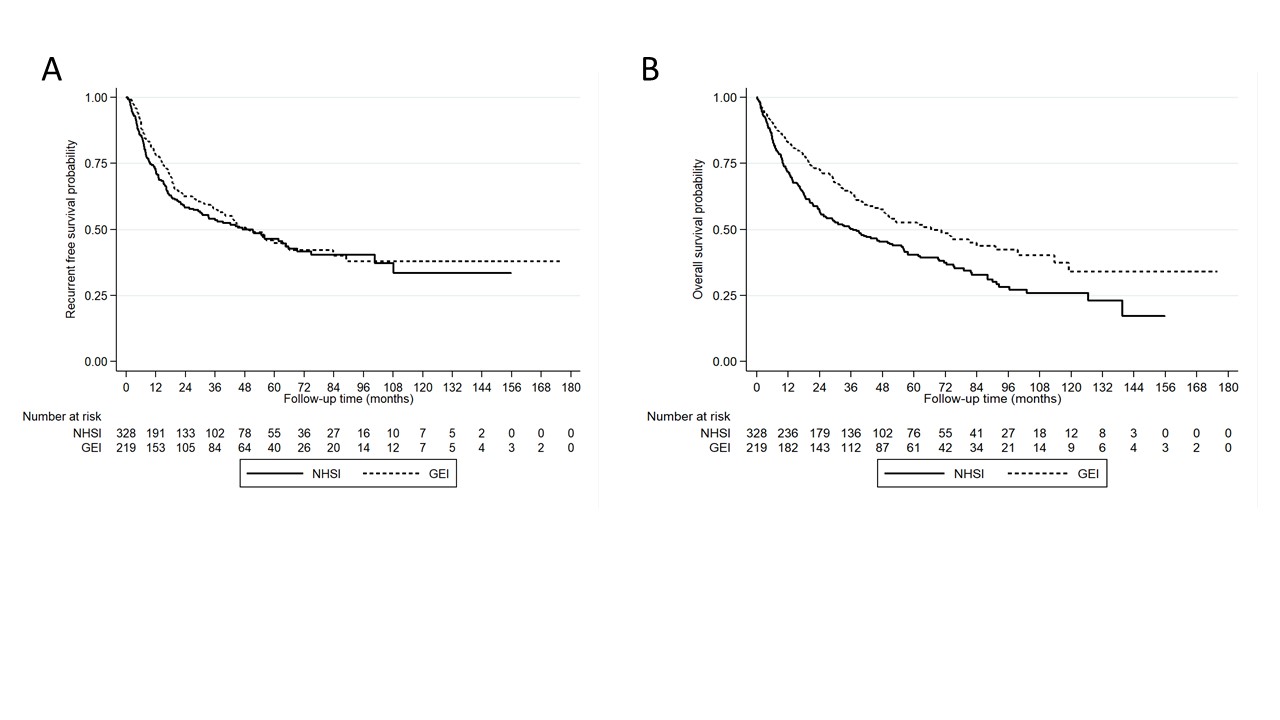
Thai NSCLC patients with NHSI coverage were more likely to experience shorter overall survival than those with GEI. The difference in medical coverage in each type of insurance, especially in term of regimens of chemotherapy, targeted therapy and immunotherapy may be associated with overall survival of patients. The Thai government should take into account this difference.
6f8b794f3246b0c1e1780bb4d4d5dc53


