Virtual Library
Start Your Search
Marcel Van Herk
Author of
-
+
MA23 - Early Stage Lung Cancer: Present and Future (ID 926)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Treatment of Early Stage/Localized Disease
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 10:30 - 12:00, Room 105
-
+
MA23.06 - Small Residual Setup Errors After Image-Guided Radiotherapy Affect Heart Dose and Are Linked to Overall Survival (ID 13785)
11:05 - 11:10 | Author(s): Marcel Van Herk
- Abstract
- Presentation
Background
There is limited evidence of the effect of radiotherapy image guidance on survival. This work investigates the relationship between small residual set-up errors following IGRT and overall survival in lung cancer patients (mostly with significant comorbidities), and explores which anatomy may be responsible for observed differences.
a9ded1e5ce5d75814730bb4caaf49419 Method
Residual setup errors of 546 NSCLC patients treated with an off-line 5mm action threshold correction protocol for bony anatomy were summarized per patient as the mean and standard deviation for each axis, as well as the vector magnitude in a direction from tumour towards the heart, and included in multivariate Cox regression. Delivered dose distributions including residual setup errors were estimated and the difference between the delivered and planned dose was compared for patients who did/did not survive longer than 1 year. Permutation testing (n=1000) assessed significance.
4c3880bb027f159e801041b1021e88e8 Result
Residual setup errors were not correlated with any pre-treatment clinical variable. Patients with a residual shift towards the heart (mean ~2 mm, max 5mm) have significantly worse overall survival (hazard ratio 1.310, p = 0.001). The average dose in the heart region changes linearly with the residual shift magnitude towards the heart (~0.8Gy/mm). A higher delivered dose than planned in a region at the heart base (Figure 1, arrow) is associated with poorer survival in multivariate analysis (hazard ratio 1.214/Gy, p<0.001).
8eea62084ca7e541d918e823422bd82e Conclusion
Small residual shifts after IGRT are strongly associated with overall survival in NSCLC patients, with shifts of the high dose region towards the heart leading to worse survival. The most likely cause of shorter survival is a corresponding increase in dose to the heart base. This analysis provides direct evidence of the importance of accurate patient positioning and highlights the significance of the heart base as a dose sensitive organ in thoracic radiotherapy patients with early effects on survival.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA01 - Improving Outcomes in Locoregional NSCLC I (ID 892)
- Event: WCLC 2018
- Type: Oral Abstract Session
- Track: Treatment of Locoregional Disease - NSCLC
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 10:30 - 12:00, Room 107
-
+
OA01.03 - Interaction Between Dose and Calcifications Is a Predictor for Overall Survival in Lung Cancer Patients Receiving Radiotherapy (ID 13920)
10:50 - 11:00 | Author(s): Marcel Van Herk
- Abstract
- Presentation
Background
Recently, incidental dose to the heart was found to be predictive for overall survival in lung cancer patients receiving radiotherapy [McWilliam et al EJC 2017, Johnson et al Radiother Oncol 2018]. These patients often present with multiple comorbidities that should be incorporated in survival analysis. However, such data is often missing. We investigated whether calcifications, identified on the radiotherapy planning CT, can be used as a surrogate for cardiac health. In particular, we investigated the interaction between calcifications, dose and survival.
a9ded1e5ce5d75814730bb4caaf49419 Method
Data from 814 unselected non-small cell lung cancer patients was used, all treated with 55Gy in 20 fractions. Methodology was developed to automatically segment calcifications within the heart, the aortic arch and their surroundings. The 3D planning CT scans, and the associated lung and spinal cord delineations were processed using well-established image processing algorithms, e.g., convex hull, thresholding, morphological operations, connected pixel analysis and flood filling to detect calcifications. Moreover, shape analysis was included to enhance regions that presented tubular or plate-like appearance. The detection algorithm was validated in a small subset of 10 patients, and this group was used to determine the success and error rate of the automatic segmentation. Finally, a Cox-proportional hazards multivariate analysis was performed for overall survival of all patients accounting for tumour size, total calcification volume, mean dose across all identified calcifications, and interaction between calcification volume and dose.
4c3880bb027f159e801041b1021e88e8 Result
The success rate of the algorithm for identifying calcifications was 81.8%, its error rate was 8.8%. The multivariate survival analysis identified tumour size (continuous, p<<0.0001) and the interaction of calcification volume and their mean dose (continuous, p=0.029) as significant. Calcification volume (p=0.57) or mean calcification radiation dose alone (p=0.269) were not found to be significant.
8eea62084ca7e541d918e823422bd82e Conclusion
Multivariate analysis shows a significant interaction between volume of the identified calcifications and their mean radiotherapy dose predicting survival. Further improvements to identify calcifications in the descending thoracic aorta and validation of our methodology are required. Further work linking our results with the established Agatston or Coronary Artery Calcium score is in progress.
* EVO-FB share first authorship
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
P1.17 - Treatment of Locoregional Disease - NSCLC (Not CME Accredited Session) (ID 949)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.17-01 - Robustness of an Image-Based Data Mining Approach in Lung Cancer Patients (ID 13384)
16:45 - 18:00 | Author(s): Marcel Van Herk
- Abstract
Background
Image-based data mining (IBDM) enables exploring the correlation of dose distributions and outcomes in large cohorts of patients without the requirement of additional contouring. IBDM has recently identified the dose to the base of the heart as an important predictor for overall survival (OS) in lung cancer patients receiving radiotherapy [McWilliam et al EJC 2017]. IBDM relies on non-rigid registration to set inter-patient dosimetric data into a common reference anatomy or reference patient. Here, we investigated the uncertainties associated with the choice of reference patient, and their influence on the correlation between incidental dose to the base of the heart and OS.
a9ded1e5ce5d75814730bb4caaf49419 Method
In previous work, 1101 NSCLC patients (55Gy / 20 fractions) were randomly selected, and their planning CT images non-rigidly registered to a reference patient CT scan using NiftyReg (http://cmictig.cs.ucl.ac.uk/wiki/) as part of IBDM process. In this work, 5 additional patients with small cell lung cancer (i.e. without a large tumour burden) were used as “reference patients” and the IBDM analysis in the whole cohort was repeated for each reference patient. Permutation testing with 100 iterations was applied to assess statistical significance.
4c3880bb027f159e801041b1021e88e8 Result

Figure 1 shows the regions of highly significant correlation between dose and OS for each reference patient. In spite of large variations in anatomy between the reference patients, each analysis identified similar anatomical regions as significantly associated with OS (t>5). Moreover, permutation testing was consistent with the original findings.
8eea62084ca7e541d918e823422bd82e Conclusion
IBDM is a robust approach and, in this analysis, does not appear to be sensitive to the choice of reference patient for the investigated dose-effect correlation. Prospective studies are necessary to confirm the correlation between dose to the base of the heart and OS in NSCLC patients. Methodological studies are needed to determine the level of effect strength and region size that this general technique can identify.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P2.01 - Advanced NSCLC (Not CME Accredited Session) (ID 950)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 2
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.01-15 - A Radiologist-Led Training Workshop for MR Based Normal Tissue and Tumour Delineation for Lung Cancer Radiotherapy. (ID 13857)
16:45 - 18:00 | Author(s): Marcel Van Herk
- Abstract
Background
A potential benefit of MR-image guided radiotherapy (MRIgRT) in lung cancer is the reduction of treatment related uncertainties through improved soft tissue contrast. However, this benefit may be obscured by inter-observer variation in gross tumour volume (GTV) and organ at risk (OAR) contouring. A radiologist led workshop was organised to provide training in such contouring on MR.
a9ded1e5ce5d75814730bb4caaf49419 Method
Planning CT, PET-CT and MRI were acquired in four lung cancer patients. MR sequences included 3D radial gradient echo, T2 DIXON Turbo Spin Echo (TSE), and T2 TSE with and without fat-sat. Data sets were local rigidly registered and imported into the so-called “Big Brother” contouring software.
The radiologist led teaching on OAR and GTV contouring used an MR lung atlas (produced by this group). Seven radiation oncologists contoured the brachial plexus (BP), heart, proximal bronchial tree, oesophagus and GTV. This was followed by a multi-disciplinary group discussion (oncologists, radiologists and physicists) on the contouring challenges and subsequently contours were reviewed and the atlas adjusted.
4c3880bb027f159e801041b1021e88e8 Result
The BP and heart were the most difficult OARs to contour and showed the largest inter-observer variation. Following contour review and discussion between radiologist and oncologists updates to atlas and protocols were made. The GTV was found to be most challenging at the soft tissue interfaces and requires further work (Figure 1).
8eea62084ca7e541d918e823422bd82e Conclusion
This early work demonstrates the need for radiologist-led training in OAR and GTV contouring in lung cancer patients using MR images. This will be especially important for the integration of MR into treatment planning and an MRIgRT adaptive workflow. We have arranged future workshops in order to provide further training and to assess inter-observer variation in OAR and GTV contouring using MR on more cases.
6f8b794f3246b0c1e1780bb4d4d5dc53 -
+
P2.01-27 - MR, CT and Cone-Beam CT for Lymph Node Visualisation in Locally-Advanced Lung Cancer (ID 11800)
16:45 - 18:00 | Author(s): Marcel Van Herk
- Abstract
Background
The largest benefit of MR-guided radiotherapy in lung cancer may be on-board visualisation of malignant lymph nodes (LNs). In this study, we assessed whether MR images were suitable for LN visualisation for treatment adaptation. We hypothesised that MR would outperform CT and Cone-Beam-CT (CBCT).
a9ded1e5ce5d75814730bb4caaf49419 Method
CT, CBCT and MR images were acquired in four lung cancer patients with malignant LNs, confirmed using PET-CT and/or endobronchial ultrasound-guided biopsies. A total of 15 LNs from mediastinal and hilar nodal stations were assessed. Imaging datasets included: (1) CT planning scan with IV contrast; (2) MR1 (within 1 week of CT); (3) Mid-treatment CBCT (without contrast); and (4) MR2 (day of CBCT). MR sequences included: Turbo Spin Echo (TSE), TSE with fat-sat and 3D radial gradient echo. The images were randomised and independently scored by four thoracic radiation oncologists according to whether the malignant LN in each nodal station was visualised well enough to permit contouring. Scores were: not visible (1), unclear (2), clear (3) and very clear (4). Scores 3 and 4 were designated as ‘suitable for contouring’.
4c3880bb027f159e801041b1021e88e8 Result
As shown in figure 1, there was no significant difference in the number of LNs deemed suitable for contouring on CT (87%) compared to MR1 (82%). A significant difference was found between CBCT (10%) and MR2 (80%).
8eea62084ca7e541d918e823422bd82e Conclusion
MR did not out-perform CT with contrast for malignant LN visualisation, possibly due to greater observer familiarity with CT. MR was significantly better than CBCT, likely due to superior soft tissue contrast. These findings support the use of MR-guided radiotherapy in locally-advanced lung cancer for adaptive planning or treatment verification. The greater variation in MR scores between oncologists (especially between sequences) could be due to lack of experience with thoracic MR. Future research will optimise MR for this task and assess LN localisation on a larger dataset.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P2.16 - Treatment of Early Stage/Localized Disease (Not CME Accredited Session) (ID 965)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 16:45 - 18:00, Exhibit Hall
-
+
P2.16-08 - Influence of Tumour Location and Histological Sub-Type of Non-Small Cell Lung Cancer on Patient Survival (ID 13836)
16:45 - 18:00 | Author(s): Marcel Van Herk
- Abstract
Background
In non-small cell lung cancer (NSCLC), adenocarcinomas tend to arise peripherally and squamous cell carcinomas (SCC) centrally. Tumour location is known to impact patient survival: in previous work, we showed that right-sided tumours show worse survival, n=1101; HR=1.25, p<0.01. In this study we extended the laterality analysis by including histological sub-type and explore its correlation with overall survival.
a9ded1e5ce5d75814730bb4caaf49419 Method
529 unselected NSCLC patients (treated with 55Gy/20fr), with confirmed adenocarcinoma or SCC, were included. All patients were spatially normalised using non-rigid registration to a reference anatomy, allowing tumour probability maps to be created from the outlined tumours. A Kolmogorov-Smirnov test assessed differences in distributions.
Kaplan-Meier curves, grouped by histological sub-type, were plotted. Tumour volumes were extracted for all patients and included in a multi-variate analysis including N-stage, performance status, gender and median dose to left and right lungs, encoding laterality.
4c3880bb027f159e801041b1021e88e8 Result
326 adenocarcinomas and 203 SCC were found. Tumour probability maps show a clear separation in tumour locations between the sub-types (Fig.1a, p<0.001) and a general location of SCC tumours along the major airways. Tumour volumes were significantly different (SCC larger, median 56cm3 versus 14cm3, p<0.001, Fig.1b). Histology also influences nodal involvement, 20% adenocarcinomas versus 80% SCC are N+. Location and volume impacts on normal tissue doses, mean lung and heart doses: 8.8Gy and 4.9Gy for adenocarcinomas, 15.6Gy and 18.8Gy for SCC.
SCC patients showed worse survival (median 12 versus 21 months, Fig.1c). Multivariate analysis shows right lung mean doses significantly correlate with survival for adenocarcinomas, p=0.04, but not for SCC, p=0.2, indicating the spatial location of the tumour may have an interaction with our previously described laterality effect.
8eea62084ca7e541d918e823422bd82e Conclusion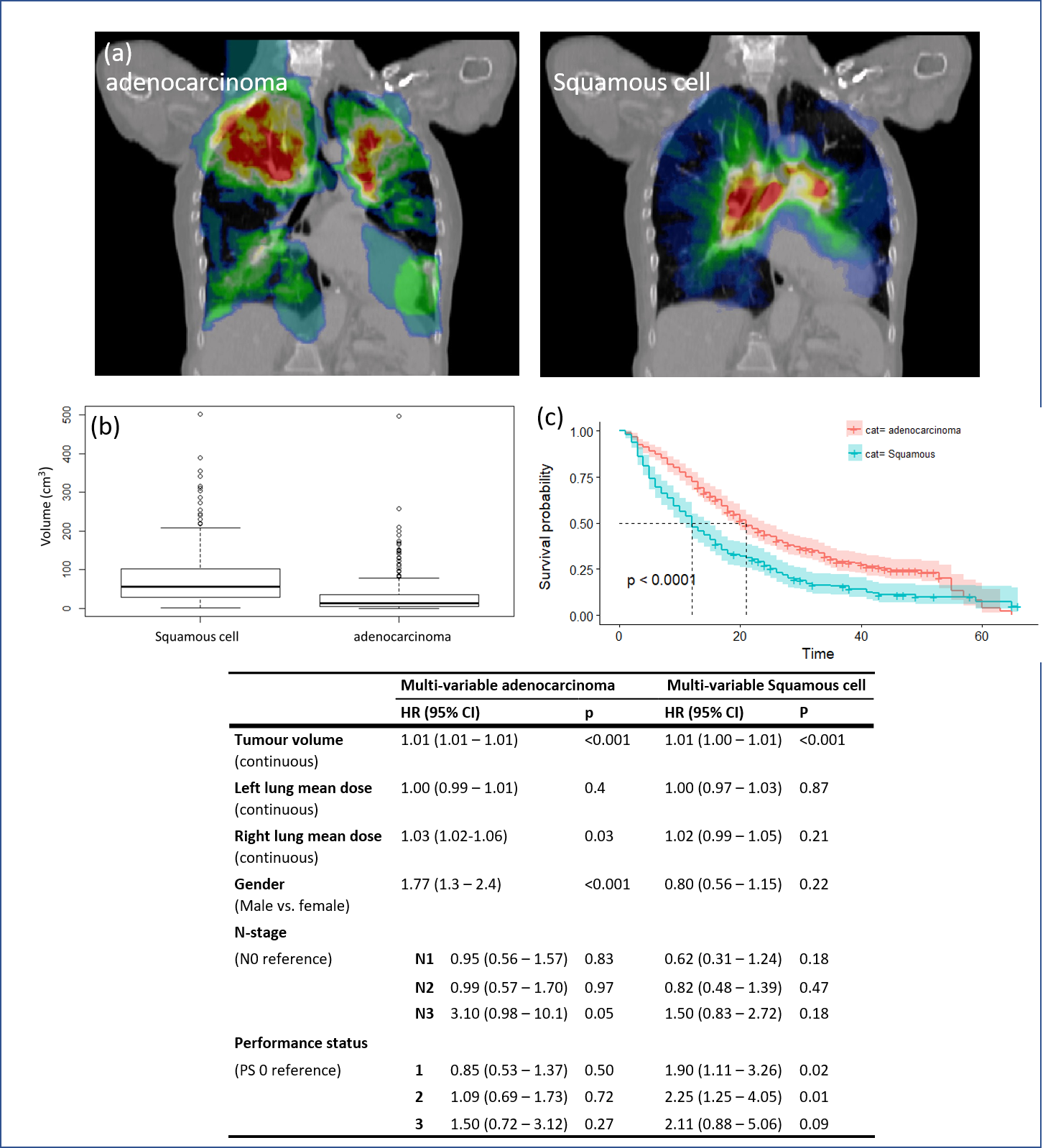
Differences in the spatial locations and volumes of histological sub-types influence normal tissue doses including the effect of tumour laterality on survival. Further work will explore possible mechanisms, including ventilation/perfusion variation in the lungs.
6f8b794f3246b0c1e1780bb4d4d5dc53


