Virtual Library
Start Your Search
Ross Camidge
Author of
-
+
MA02 - Improving Outcomes for Patients with Lung Cancer (ID 895)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Advanced NSCLC
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 10:30 - 12:00, Room 201 BD
-
+
MA02.01 - ROS1 Gene Rearrangements Are Associated with an Exaggerated Risk of Peri-Diagnosis Thromboembolic Events (ID 12442)
10:30 - 10:35 | Author(s): Ross Camidge
- Abstract
- Presentation
Background
Based on clinical observation, we hypothesized that ROS1 gene-rearranged non-small cell lung cancer (ROS1+ NSCLC) has a higher than expected thromboembolic event (TEE) rate. A multicenter, retrospective cohort study of TEE in advanced ROS1+, KRAS+, ALK+ and EGFR+ NSCLC was conducted.
a9ded1e5ce5d75814730bb4caaf49419 Method
Venous (DVT / PE) and arterial (MI/TIA/CVA) TEE within +/- 365 days of diagnosis of ROS1+, KRAS+, ALK+ or EGFR+ advanced NSCLC at 4 academic centers in USA and China from October 2002 to January 2018 were captured. The primary endpoint was the incidence of TEE in ROS1+ compared to KRAS+ NSCLC as a control group within +/- 90 days of diagnosis. Secondary endpoints compared TEE incidence between ROS1+ and ALK+, and ROS1+ and EGFR+. Fine-Gray Model was used to detect differences in TEE incidence while accounting for death as a competing risk.
4c3880bb027f159e801041b1021e88e8 Result
105 ROS1+, 101 ALK+, 112 EGFR+, and 114 KRAS+ NSCLC patients were enrolled. Incidence rate of TEE within +/- 90 days of diagnosis was 30.5% (32/105), 12.9% (13/101), 7.1% (8/112), and 12.3% (14/114) in the respective molecular cohorts. Compared to the ROS1+ cohort, the risk of TEE was significantly lower in the three other cohorts (KRAS+ HR 0.334, 95% CI: 0.18-0.62, p=0.001; ALK+ HR 0.357, 95% CI: 0.188-0.68, p=0.002; EGFR+ HR 0.193, 95% CI: 0.089-0.421, p<0.001) (Figure 1). First event TEEs were venous as opposed to arterial in 59.5% (22/37) ROS1+, 87.1% (27/31) ALK+, 80.6% (25/31) EGFR+, and 80% (16/20) KRAS+ cases. The median time (Interquartile Range) to TEE from the time of diagnosis for ROS1+/ALK+/EGFR+/ KRAS+ was 0 days (-6.75 to 7.0), 0 days (-20.0 to 35.0), 0.50 days (-43.7 to 21.3), and 13 days (0.49 to 32.0), respectively.
8eea62084ca7e541d918e823422bd82e Conclusion
Among common molecular subtypes of NSCLC, ROS1+ oncogene is associated with a significantly higher risk of developing TEE within +/- 90 days of advanced NSCLC diagnosis.
6f8b794f3246b0c1e1780bb4d4d5dc53
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
MA04 - Novel Approaches with IO (ID 900)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Immunooncology
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 13:30 - 15:00, Room 107
-
+
MA04.03 - Immunotherapy for Non-Small Cell Lung Cancers (NSCLC) with Oncogenic Driver Mutations: New Results from the Global IMMUNOTARGET Registry (ID 13187)
13:40 - 13:45 | Author(s): Ross Camidge
- Abstract
- Presentation
Background
Prospective data on immunotherapy for NSCLC with oncogenic driver mutations are limited. We recently reported first results from the global IMMUNOTARGET registry (Mazières, ASCO 2018). Here, we present new data for PD-L1 and mutation subgroups.
a9ded1e5ce5d75814730bb4caaf49419 Method
In 2017, we started an international retrospective registry study ("IMMUNOTARGET") for patients with advanced NSCLC, known driver mutations (KRAS, EGFR, ALK, ROS1, BRAF, HER2, MET and RET) and PD-L1 immune checkpoint inhibitor therapy. The registry is approved by University of Toulouse and Swissethics, and funded by University of Toulouse and Cantonal Hospital of Lucerne. Anonymized real-world data submitted to the coordinating center include: patient and tumor characteristics, mutation test methods and results, systemic therapy lines, immune related adverse events, best response by RECIST, survival, and tumor PD-L1 expression (optional). Statistical calculations including best response, median PFS and OS are done at University of Toulouse.
4c3880bb027f159e801041b1021e88e8 Result
In April 2018, the registry included 551 pts from Europe, USA, Israel and Australia. Patients were 50% male/female, 28% current smokers, median age 60 years (range 28-83), 85% had PS0/1. Most (73%) tumors were stage IV at diagnosis, almost all (96%) were adenocarcinomas. Molecular classification by dominant driver mutation: KRAS=271 (49%), EGFR=125 (23%), BRAF=43 (8%), MET=36 (7%), HER2=29 (5%), ALK=23 (4%), RET=16 (3%), ROS1=7 (1%), 1 (0.2%) not classified (ALK+RET+MET). Most pts received nivolumab (466) or pembrolizumab (48) and were treated with immunotherapy in second or third line (67%). The median number of cycles was 5 (range 1-68). Fifty (11%) pts had grade 3-5 toxicity. Median OS from start of immunotherapy was 13.3 months, median PFS was 2.8 months. Best response was PR/CR in: KRAS=26%, BRAF=24%, ROS1=17%, MET=16%, EGFR=12%, HER2=7%, RET=6%, ALK=0%. Percentage of PD-L1 positive cells was available for 177 pts: 0%=71 (40%), 1-49%=46 (26%), 50-100%=60 (34%). Median % of positive cells was highest for ROS1 (90%), BRAF (50%), MET (30%) and RET (26%) mutant tumors. PD-L1 positivity was predictive for improved PFS in KRAS and EGFR mutant tumors. PD-L1 status was known in 18 tumors with ALK, ROS1 or RET rearrangements: 5 had 0%, 4 had 1-49% and 9 had 50%-100%. No tumor remissions were observed in this subgroup. The registry remains open, updated results will be presented at the conference.
8eea62084ca7e541d918e823422bd82e Conclusion
Although response rates were lower than in KRAS mutant NSCLC, individual tumors with other driver mutations responded to immunotherapy. PD-L1 expression may not accurately predict clinical benefit from immunotherapy in some molecular subgroups, better markers are needed.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
MA16 - Novel Mechanisms for Molecular Profiling (ID 917)
- Event: WCLC 2018
- Type: Mini Oral Abstract Session
- Track: Advanced NSCLC
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 13:30 - 15:00, Room 203 BD
-
+
MA16.02 - Prospective Clinical Validation of the InVisionFirst™ ctDNA Assay for Molecular Profiling of Patients with Advanced NSCLC (ID 13885)
13:35 - 13:40 | Author(s): Ross Camidge
- Abstract
- Presentation
Background
Clinical practice guidelines advocate molecular profiling as a part of the evaluation of advanced NSCLC, with ctDNA based profiling being an option for those with insufficient tissue. Thorough prospective clinical validation studies of NGS based ctDNA assays are lacking. Here we report the multi-centered prospective clinical validation of a ctDNA NGS panel for stratification of patients with advanced untreated NSCLC.
a9ded1e5ce5d75814730bb4caaf49419 Method
InVisionFirst™ (Inivata) is a ctDNA NGS assay for detection of genomic alterations in 36 genes commonly mutated in NSCLC and other cancers. 264 patients with untreated advanced NSCLC were prospectively recruited by 41 US centers. 178 patients had tumour tissue available for molecular profiling (predominantly by NGS) and the remaining 86 patients without tissue were included to compare ctDNA profiles obtained from patients with and without tissue for profiling.
4c3880bb027f159e801041b1021e88e8 Result
A total of 204 patients (77.3%) had detectable ctDNA alterations. Using tissue results as the reference, overall concordance for the full 36 genes in the InVisionFirst™ panel with matched tissue profiling was 97.8% with 82.9% PPV, 98.5% NPV, 70.6% sensitivity and 99.2% specificity. Considering a subgroup of 8 genes that can influence routine clinical patient management (EGFR, ALK, ROS1, ERBB2, MET, BRAF, KRAS, STK11) the PPV was 93.7%, 96.8% NPV, 72.4% sensitivity and 99.4% specificity. Excluding patients with undetectable ctDNA, these figures become 93.7% PPV, 98.4% NPV, 87.3% sensitivity and 99.3% specificity. The observed pattern of genomic changes seen in ctDNA was consistent across patients with and without tissue for profiling. Across the whole study, 44 patients with actionable alterations were identified by ctDNA testing compared to only 36 by tissue testing. 47% of patients tested by ctDNA had an actionable alteration or an alteration that is generally mutually exclusive for such actionable changes such as KRAS or STK11.
8eea62084ca7e541d918e823422bd82e Conclusion
The InVisionFirst™ assay demonstrates excellent concordance with tissue profiling in this multi-centered prospective clinical validation study. The performance of this assay in terms of overall sensitivity and specificity appears comparable if not higher than other established commercial ctDNA assays. Utilization of InVisionFirst™ ctDNA testing led to the detection of 22% more actionable alterations than standard of care tissue testing in this study supporting its use for the molecular stratification of patients with advanced NSCLC. Further analyses on the features associated with detectable ctDNA signatures are ongoing.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
MS06 - Practical Issues in the Management of Oligometastatic NSCLC (ID 785)
- Event: WCLC 2018
- Type: Mini Symposium
- Track: Oligometastatic NSCLC
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 13:30 - 15:00, Room 206 BD
-
+
MS06.04 - Systemic Therapy for Oligomets: Before, During, or After Local Therapies? (ID 11426)
14:15 - 14:30 | Presenting Author(s): Ross Camidge
- Abstract
- Presentation
Abstract not provided
Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA02 - Novel Therapies in ROS1, HER2 and EGFR (ID 893)
- Event: WCLC 2018
- Type: Oral Abstract Session
- Track: Targeted Therapy
- Presentations: 1
- Moderators:
- Coordinates: 9/24/2018, 10:30 - 12:00, Room 105
-
+
OA02.02 - Safety and Preliminary Clinical Activity of Ropotrectinib (TPX-0005), a ROS1/TRK/ALK Inhibitor, in Advanced ROS1 Fusion-Positive NSCLC (ID 14217)
10:40 - 10:50 | Author(s): Ross Camidge
- Abstract
- Presentation
Background
Ropotrectinib is a potent ROS1/TRK/ALK inhibitor with a >90-fold greater ROS1 potency than crizotinib. Preclinical studies demonstrate robust activity against all known ROS1 resistance mutations, including solvent-front mutation G2032R.
a9ded1e5ce5d75814730bb4caaf49419 Method
In this Phase 1 study (NCT03093116), TKI-naïve and TKI-refractory (≥1 TKI) pts with advanced ALK/ROS1/TRK+ solid tumors received ropotrectinib. Asymptomatic brain metastases were allowed. Primary objectives were to determine MTD and RP2D, with safety, pharmacokinetics, and preliminary antitumor efficacy as the secondary objectives. This is a safety analysis of all pts and subgroup efficacy analysis of the ROS1+ NSCLC pts on the study.
4c3880bb027f159e801041b1021e88e8 Result
As of 16-April-2018, 72 pts have been treated at 6 dose levels from 40mg QD to 200mg BID. Most AEs were grade 1-2. Common (>10%) treatment-related AEs included dizziness (49%), dysgeusia (46%), paresthesias (29%), constipation (19%), fatigue (18%), nausea (11%), and anemia (11%). 4 DLTs were observed at ≥240mg/day: 1 grade 3 (Gr3) dyspnea/hypoxia, 2 Gr3 & 1 Gr2 dizziness. 31 of 72 pts had ROS1+ NSCLC by local testing (FISH, n=20; NGS, n=11) with 1 pt determined as ROS1-negative by central NGS. Antitumor activity in ROS1+ NSCLC has been observed at ROS1 dose levels 40mg QD-160mg BID per investigator assessment, with the best ORR 70% for TKI-naïve and 11% for TKI-refractory pts (17% for 1 prior TKI crizotinib, n=12) (Table). Two crizotinib-resistant pts with G2032R achieved durable cPR and cSD, respectively. Ongoing blinded independent review identified 7 evaluable pts with target CNS lesions at baseline; the intracranial best ORR was 43% (3 cPR, 1 PR*). Updated efficacy data and ctDNA biomarker analyses will be presented.
8eea62084ca7e541d918e823422bd82e ConclusionDose Level
TKI Naïve (n = 10)
TKI Refractory (n = 20)
n
Best Overall Response
n
Best Overall Response
40 mg QD (n = 6)
2
2 cPR (ORR 100%)
4
2 cSD, 1 SD, 1 PD
80 mg QD (n = 5)
2
2 cPR (ORR 100%)
3
1 cSD, 2 SD
160 mg QD (n = 10)
4
2 cPR, 2 cSD (ORR 50%)
6
2 cPR, 2 cSD, 1 SD, 1 PD (ORR 33%)
240 mg QD (n = 2)
1
1 cPR (ORR 100%)
1
1 SD
160 mg BID (n = 7)
1
1 PR*
6
1 PR*, 1 SD*, 1 cSD, 2 SD, 1 NE
Total (n = 30)
10
7 cPR, 1 PR*, 2 cSD
20
2 cPR, 1 PR*, 6 cSD, 1 SD*, 7 SD, 2 PD, 1 NE
Best ORR
70%
11%
Median follow-up
8 months with 90% still on treatment
4 months with 50% still on treatment
cPR: confirmed partial response; SD: stable disease for 2 cycles; cSD: SD for at least 4 cycles; PR* or SD*: waiting for subsequent time point scan; PD: progressive disease; NE: inevaluable; ORR: objective response rate
Ropotrectinib is well tolerated and demonstrates promising activity in pts with advanced ROS1+ NSCLC, including TKI-naïve and TKI-refractory pts. RP2D has not yet been achieved. These Phase 1 data warrant further clinical testing of ropotrectinib in ROS1+ NSCLC.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA12 - Novel Therapies in MET, RET and BRAF (ID 921)
- Event: WCLC 2018
- Type: Oral Abstract Session
- Track: Targeted Therapy
- Presentations: 2
- Moderators:
- Coordinates: 9/25/2018, 15:15 - 16:45, Room 106
-
+
OA12.02 - Updated Antitumor Activity of Crizotinib in Patients with MET Exon 14-Altered Advanced Non-Small Cell Lung Cancer (ID 13453)
15:25 - 15:35 | Author(s): Ross Camidge
- Abstract
- Presentation
Background
MET exon 14 alterations occur in ~3% of non-squamous non-small cell lung cancer (NSCLCs) and 20–30% of sarcomatoid lung carcinomas. Here we present updated antitumor activity for crizotinib in patients with advanced NSCLC whose tumors are positive for MET exon 14 alterations (hereafter MET exon 14-positive NSCLC), including updated biomarker analyses in circulating tumor DNA (ctDNA).
a9ded1e5ce5d75814730bb4caaf49419 Method
Patients with MET exon 14-positive NSCLC by local molecular profiling were treated with 250 mg crizotinib BID in an expansion cohort of the ongoing PROFILE 1001 study (NCT00585195). Responses were based on derived investigator assessment per RECIST v1.0. Prospective plasma profiling for MET exon 14 alterations in plasma ctDNA was performed (PlasmaSELECT-R64; Personal Genome Diagnostics, Boston, MA).
4c3880bb027f159e801041b1021e88e8 Result
As of Jan 31, 2018, 69 patients (65 response-evaluable) with MET exon 14-positive NSCLC had been treated. Median age was 72 y (range: 34, 91). Tumor histology was: 84% adenocarcinoma, 9% sarcomatoid adenocarcinoma, 4% squamous cell carcinoma and 3% adenosquamous carcinoma. 61% were former-smokers, 38% never-smokers and 1% a current smoker. Median duration of treatment was 7.4 mo (95% CI: 5.5, 9.1), with 29% of patients ongoing. Confirmed responses were 3 CRs and 18 PRs (ORR, 32% [95% CI: 21, 45]); 29 patients had SD as their best overall response (Figure).
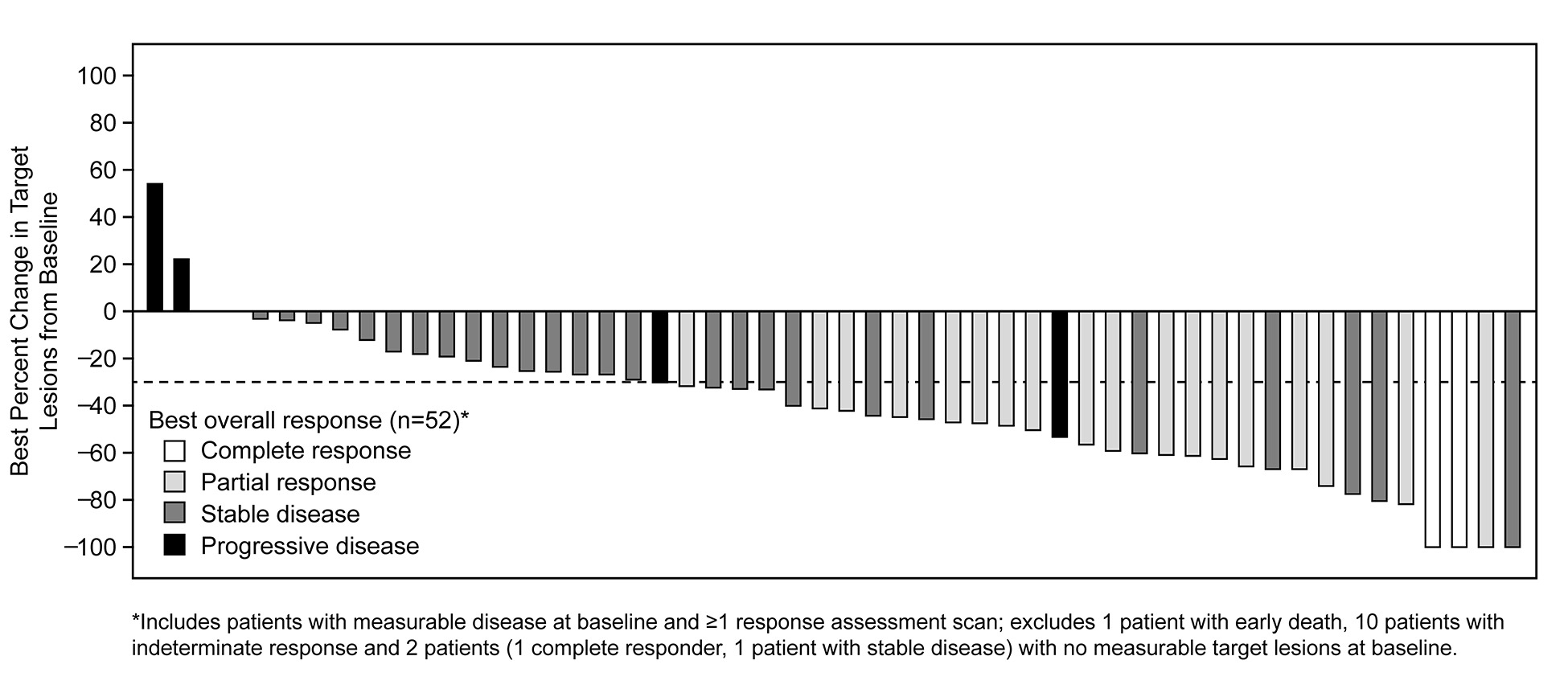
Median time to response was 7.6 weeks (range: 3.7, 16.3). Median DOR was 9.1 mo (95% CI: 6.4, 12.7). Median PFS was 7.3 mo (95% CI: 5.4, 9.1). MET exon 14 alterations were detected in ctDNA from 18/37 (49%) patients with analyzable samples.
8eea62084ca7e541d918e823422bd82e Conclusion
In patients with MET exon 14-positive advanced NSCLC, crizotinib treatment led to objective responses that were rapid and durable, with CRs in some cases. Plasma ctDNA profiling detected MET exon 14 alterations in a subset of patients who harbor MET exon 14 alterations by tumor testing.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
OA12.06 - Mutational Landscape of BRAF V600E Positive Lung Cancer Patients Following BRAF Directed Therapy Failure (ID 13540)
16:10 - 16:20 | Author(s): Ross Camidge
- Abstract
- Presentation
Background
BRAF V600E mutation is identified as molecular drivers in 1-2% of lung adenocarcinomas and predicts response to combination BRAF and MEK inhibitors. Little is known about molecular mechanisms of acquired resistance to these therapies for lung cancer patients with BRAF V600E mutations, partially due to a lack of representative cancer models.
a9ded1e5ce5d75814730bb4caaf49419 Method
We identified patients with BRAF V600E mutated lung cancer who were progressing after initial response to a BRAF/MEK inhibitor combination in 5 academic institutions in the US. Potential molecular mechanisms of resistance were explored by comparing pre- and post-therapy results from comprehensive tissue and/or the Guardant360 and FoundationACT plasma-based next generation sequencing assays.
4c3880bb027f159e801041b1021e88e8 Result
We identified 6 patients. Prior to treatment with a BRAF/MEK inhibitor combination, four patients had received at least one line of chemotherapy and immune checkpoint inhibitor monotherapy, one had received chemotherapy only and one was treatment naïve. Five patients received dabrafenib/trametinib and one vemurafenib/cobimetinib combination. All 6 patients achieved a partial response. Progression free survival (PFS) ranged from 3 to 15 months (median 9.5 months). At the time of progression, all patients had the BRAF V600E mutation re-identified in their samples. Additionally, there was one patient with a new AKT1 E17K and a new KRAS G12A mutation, one patient with a new VHL R167Q mutation and one patient with a new TP53 splice site indel mutation at the time of progression. Another two patients had AKT1 E17K mutations that were present prior to BRAF/MEK inhibitor therapy. They both had oligoprogression, one in lymph nodes and one in the brain after 5.2 and 3 months, respectively; both continued on dabrafenib and trametinib combination therapy after radiation treatment to the progressing sites. Interestingly, co-occurrence of AKT1 E17K and BRAF V600E mutations is rare in the TCGA data, but was identified in three of six patients in our case series. Finally, we have established a BRAF V600E positive lung adenocarcinoma cell line from a TKI naïve patient for further functional studies of drug resistance.
8eea62084ca7e541d918e823422bd82e Conclusion
Comprehensive molecular testing can identify potential resistance mechanisms following progression of BRAF V600E positive lung cancer to TKI therapy. AKT1 mutations were common as co-alterations in BRAF V600E mutated lung adenocarcinoma before and after targeted therapy and may contribute to drug resistance. The development of patient-derived cell line models may assist in the identification and validation of drug resistance mechanisms, and may help devise strategies to overcome drug resistance.
6f8b794f3246b0c1e1780bb4d4d5dc53Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.
-
+
P1.01 - Advanced NSCLC (Not CME Accredited Session) (ID 933)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 2
- Moderators:
- Coordinates: 9/24/2018, 16:45 - 18:00, Exhibit Hall
-
+
P1.01-62 - The Third Generation Irreversible EGFR Inhibitor HS-10296 in Advanced Non-Small Cell Lung Cancer Patients (ID 13138)
16:45 - 18:00 | Author(s): Ross Camidge
- Abstract
Background
The epidermal growth factor receptor (EGFR) T790M mutation is the most common mechanism of drug resistance to EGFR tyrosine kinase inhibitors (TKIs) in non-small cell lung cancer (NSCLC) patients with sensitizing EGFR mutations. The third generation irreversible EGFR inhibitor HS-10296 has been shown to be safe and effective against both EGFR TKI-sensitizing and T790M resistance mutations in preclinical studies.
a9ded1e5ce5d75814730bb4caaf49419 Method
A Phase I, open-label, multi-center clinical trial was conducted in patients with locally advanced or distant metastatic NSCLC who have progressed following prior therapy with EGFR TKIs. The study was consisted of dose-escalation cohorts (55, 110, 220 and 260 mg) and dose-expansion cohorts (55, 110 and 220 mg) with once daily oral administration of HS-10296. In each expansion cohort, tumor biopsies were collected for central determination of EGFR T790M status. Patients were assessed for safety, tolerability, pharmacokinetics and efficacy of HS-10296.
4c3880bb027f159e801041b1021e88e8 Result
A total of 117 patients (median age 60) received at least one dose of HS-10296 across multiple sites in China (43 patients), Taiwan (69 patients) and the United States (5 patients). Maximum tolerated dose(MTD)has not been reached in this study. The most common adverse events were grade1/2 rash, pyrexia, upper respiratory tract infection, constipation, diarrhoea and blood creatine phosphokinase elevation. Drug-related serious adverse events were anemia (0.8%), blood creatinine elevation (0.8%), anemiarhabdomyolysis (0.8%) and blood creatine phosphokinase elevation (0.8%) occurred mainly in the cohorts with higher doses at 220 mg or 260 mg, respectively. These data demonstrated favorable tolerability and safety of HS-10296 in patients enrolled. The pharmacokinetics of HS-10296 was dose proportional and the plasma half-life was 30.7~37.5 hours. Among 82 evaluable patients (18 in escalation cohorts and 64 in expansion cohorts) with the EGFR T790M mutation, the overall objective response rate (ORR) was 52.4% (43/82; 95% CI, 41.6 to 63.3), while disease control rate (DCR) was 91.5% (75/82; 95% CI, 85.4 to 97.5). 110mg cohort showed better DCR (97.2% VS. 86.1%) than 55mg cohort. Phase II study is ongoing with the dose at 110 mg.
8eea62084ca7e541d918e823422bd82e Conclusion
HS-10296 has the potential to provide clinical benefit to locally advanced or distant metastatic NSCLC patients with EGFR T790M mutation who had disease progression following prior therapy with EGFR TKIs.
(The study was sponsored by Jiangsu Hansoh Pharmaceutical Co., Ltd.; ClinicalTrials.gov number, NCT02981108)
6f8b794f3246b0c1e1780bb4d4d5dc53 -
+
P1.01-78 - The Incidence of Brain Metastases in ROS1-Rearranged Non-Small Cell Lung Cancer at Diagnosis and Following Progression on Crizotinib (ID 14164)
16:45 - 18:00 | Author(s): Ross Camidge
- Abstract
Background
Central nervous system (CNS) metastases in lung cancer are a frequent cause of morbidity and mortality. There are conflicting data on the incidence of CNS metastases in ROS1+ NSCLC at diagnosis and rate of CNS progression on crizotinib.
a9ded1e5ce5d75814730bb4caaf49419 Method
Retrospective review of 579 patients with stage IV NSCLC between June 2008 to December 2017 was performed. We captured presence of brain metastases and oncogene status. We measured progression free survival (PFS) and time to CNS progression in ROS1+ and ALK+ patients on crizotinib.
4c3880bb027f159e801041b1021e88e8 Result
We identified 33 ROS1+ and 115 ALK+ patients with advanced NSCLC. The incidence of brain metastases for treatment-naïve ROS1+ and ALK+ NSCLC was 36% (12/33) and 34% (39/115) respectively. There were no statistically significant differences in incidence of brain metastases across all oncogene sub-groups. Complete survival data was available for 19 ROS1+ and 83 ALK+ patients. Median PFS for the ROS1+ and ALK+ cohort was 11 and 8 months (p = 0.304). The CNS was the first site of progression for 52% (10/19) ROS1+ NSCLC and 43% (36/83) ALK+ NSCLC with no significant differences between the groups (p = 0.610). Among patients without CNS metastases prior to crizotinib therapy, 50% of ROS1+ and ALK+ patients developed CNS metastases as only site of progression at 24 and 21 months respectively.
8eea62084ca7e541d918e823422bd82e Conclusion
Brain metastases are common in treatment-naïve stage IV ROS1+ NSCLC, though incidence does not differ from other oncogene cohorts. The CNS is a common first site of progression in patients with ROS1+ NSCLC on crizotinib. This study reinforces the need to develop CNS-penetrant TKIs for patients with ROS1+ NSCLC, similar to ALK+ NSCLC.
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
P3.04 - Immunooncology (Not CME Accredited Session) (ID 970)
- Event: WCLC 2018
- Type: Poster Viewing in the Exhibit Hall
- Track:
- Presentations: 1
- Moderators:
- Coordinates: 9/26/2018, 12:00 - 13:30, Exhibit Hall
-
+
P3.04-23 - Phase 1b/2 Study to Evaluate Novel Combinations With Oleclumab (MEDI9447) in Previously Treated Advanced EGFRm NSCLC (ID 12300)
12:00 - 13:30 | Author(s): Ross Camidge
- Abstract
Background
Patients with mutant EGFR (EGFRm) non–small cell lung cancer (NSCLC) have a limited chance of benefiting from treatment with programmed death-1 inhibitors. EGFR activation leads to overexpression of CD73 and may provide a mechanism of immune evasion. CD73 overexpression has also led to worse outcomes in multiple tumor types, including NSCLC. Recent studies demonstrated that an orthogonal therapeutic approach to cancer, such as combining tyrosine kinase inhibitors (TKIs) with immunotherapy, may result in synergistic clinical activity. Oleclumab is a human monoclonal antibody (mAb) that selectively binds to CD73 and inhibits the enzymatic production of adenosine. Adenosine exerts its immunosuppressive effects on various immune cells via the adenosine 2A receptor (A2AR). AZD4635 is a potent, selective A2AR antagonist that inhibits this signaling pathway. Osimertinib is a potent and selective inhibitor of EGFRm, including the T790M resistance mutation. We hypothesize that novel combinations of targeted and immunotherapeutic agents targeting the adenosine pathway will be well tolerated and lead to increased antitumor activity in subjects with EGFRm NSCLC.
a9ded1e5ce5d75814730bb4caaf49419 Method
This is a multi-arm, open-label, multicenter, phase 1b/2 study (NCT03381274) consisting of 2 parts. In Part 1, the safety and tolerability of oleclumab in combination with either osimertinib (Arm A) or AZD4635 (Arm B) will be evaluated, and a recommended phase 2 dose for each combination will be identified. In Part 2, the safety, tolerability, and preliminary antitumor activity will be evaluated. In both parts, patients will be allocated to treatment arms based upon their EGFRm status and their prior therapy. For Part 2, the primary objective of antitumor activity will be assessed by objective response according to RECIST v1.1. Key secondary objectives include additional evaluation of clinical activity, the pharmacokinetic profiles of oleclumab, osimertinib, and AZD4635, and the evaluation of oleclumab immunogenicity. Additional treatment arms may be added as the study progresses. The study is open for enrollment and recruitment is ongoing, with a planned enrollment of up to approximately 98 patients.
4c3880bb027f159e801041b1021e88e8 Result
Section not applicable
8eea62084ca7e541d918e823422bd82e Conclusion
Section not applicable
6f8b794f3246b0c1e1780bb4d4d5dc53
-
+
PL02 - Presidential Symposium - Top 5 Abstracts (ID 850)
- Event: WCLC 2018
- Type: Plenary Session
- Track: Advanced NSCLC
- Presentations: 1
- Moderators:
- Coordinates: 9/25/2018, 08:15 - 09:45, Plenary Hall
-
+
PL02.03 - Brigatinib vs Crizotinib in Patients With ALK Inhibitor-Naive Advanced ALK+ NSCLC: First Report of a Phase 3 Trial (ALTA-1L) (ID 11155)
08:30 - 08:40 | Presenting Author(s): Ross Camidge
- Abstract
- Presentation
Background
Brigatinib has robust efficacy in crizotinib-resistant ALK+ NSCLC, exhibiting median progression-free survival (mPFS) of 16.7 months. We report results of the first interim analysis from the ALTA-1L study of brigatinib vs crizotinib in ALK TKI-naive, ALK+ NSCLC (NCT02737501).
This open-label, multicenter study enrolled patients with stage IIIB/IV ALK+ NSCLC based on local ALK testing (FDA approved/other). Eligible patients had ECOG PS 0–2, ≤1 prior systemic therapy for locally advanced/metastatic NSCLC, and no prior ALK inhibitor. Asymptomatic CNS metastases were allowed. All patients had systematic CNS imaging. Patients were randomized 1:1 to brigatinib 180 mg QD with 7-day lead-in at 90 mg or crizotinib 250 mg BID. Primary endpoint: blinded independent review committee (BIRC)-assessed PFS (RECIST v1.1). Secondary efficacy endpoints included BIRC-assessed objective response rate (ORR), intracranial ORR (iORR), and intracranial PFS (iPFS). Interim analyses were planned at 50% and 75% of planned PFS events (n=198).
275 patients were randomized (brigatinib/crizotinib, n=137/138); median age (years) 58/60. 26%/27% received prior chemotherapy for advanced disease, and 29%/30% had baseline brain metastases. At data cut-off (19 February 2018), median follow-up brigatinib/crizotinib: 11.0/9.25 months; with 99 PFS events, brigatinib met the prespecified threshold for statistical superiority vs crizotinib in the primary endpoint, BIRC-assessed PFS (HR 0.49, 95% CI 0.33–0.74, log-rank P=0.0007); brigatinib mPFS was not reached (95% CI NR–NR) vs crizotinib 9.8 months (95% CI 9.0–12.9). Investigator-assessed PFS HR 0.45 (95% CI 0.30–0.68), log-rank P=0.0001. Table shows additional efficacy data. Most common treatment-emergent AEs grade ≥3: brigatinib: increased CPK (16.2%), increased lipase (13.2%), hypertension (9.6%); crizotinib: increased ALT (9.5%), AST (5.8%), and lipase (5.1%). Any grade ILD/pneumonitis: brigatinib, 3.7%; crizotinib, 2.2%. Discontinuations due to AE (brigatinib/crizotinib): 11.8%/8.8%.
Brigatinib showed a statistically and clinically significant improvement in PFS compared with crizotinib in ALK inhibitor–naive ALK+ NSCLC.
BIRC-Assessed Endpoint, % Brigatinib
(n=137)
Crizotinib
(n=138)
P-Value All patients ORRa 76 (68–83b) 73 (65–80b) Confirmed ORR 71 (62–78b) 60 (51–68b) 0.0678 With any intracranial CNS metastases (n=43) (n=47) iORRa 79 (64–90b) 23 (12–38b) Confirmed iORR 67 (51–81b) 17 (8–31b) <0.0001 Median iPFS, months NR (11–NRb) 6 (4–9b) 1-year iPFS 67 (47–80b) 21 (6–42b) HR 0.27 (0.13–0.54) <0.0001c With measurable intracranial CNS metastases (n=18) (n=21) iORRa 83 (59–96b) 33 (15–57b) Confirmed iORR 78 (52–94b) 29 (11–52b) 0.0028 aResponse, ≥1 assessment; b95% CI; cLog-rank.
a9ded1e5ce5d75814730bb4caaf49419Only Members that have purchased this event or have registered via an access code will be able to view this content. To view this presentation, please login, select "Add to Cart" and proceed to checkout. If you would like to become a member of IASLC, please click here.


